FALSE000133349300013334932024-02-272024-02-27
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
WASHINGTON, D.C. 20549
FORM 8-K
CURRENT REPORT
PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934
Date of Report (date of earliest event reported): February 27, 2024
EHEALTH, INC.
(Exact Name of Registrant as Specified in its Charter) | | | | | | | | |
| | |
| Delaware | 001-33071 | 56-2357876 |
| (State or other jurisdiction of incorporation) | (Commission File Number) | (I.R.S. Employer Identification No.) |
13620 RANCH ROAD 620 N, SUITE A250
AUSTIN, TX 78717
(Address of principal executive offices) (Zip Code)
(737) 248-2340
(Registrant’s telephone number, including area code)
Not applicable
(Former name or former address, if changed since last report.)
Check the appropriate box below if the Form 8-K filing is intended to simultaneously satisfy the filing obligation of the registrant under any of the following provisions:
☐ Written communications pursuant to Rule 425 under the Securities Act (17 CFR 230.425)
☐ Soliciting material pursuant to Rule 14a-12 under the Exchange Act (17 CFR 240.14a-12)
☐ Pre-commencement communications pursuant to Rule 14d-2(b) under the Exchange Act (17 CFR 240.14d-2(b))
☐ Pre-commencement communications pursuant to Rule 13e-4(c) under the Exchange Act (17 CFR 240.13e-4(c))
Securities registered pursuant to Section 12(b) of the Act: | | | | | | | | | | | | | | |
| Title of each class | | Trading Symbol(s) | | Name of each exchange on which registered |
| Common Stock, par value $0.001 per share | | EHTH | | The Nasdaq Stock Market LLC |
Indicate by check mark whether the registrant is an emerging growth company as defined in Rule 405 of the Securities Act of 1933 (17 CFR §230.405) or Rule 12b-2 of the Securities Exchange Act of 1934 (17 CFR §240.12b-2). Emerging growth company ☐
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ¨
| | | | | | | | |
| Item 2.02 | | Results of Operations and Financial Condition. |
On February 27, 2024, eHealth, Inc. (the “Company”) issued a press release announcing its financial results for the fourth quarter and fiscal year ended December 31, 2023 and its financial condition as of December 31, 2023. A copy of the press release is furnished as Exhibit 99.1 to this Current Report on Form 8-K and is incorporated herein by reference.
On February 27, 2024, the Company posted supplemental investor material on its investor relations webpage at https://ir.ehealthinsurance.com. The Company intends to use its investor relations webpage as a means of disclosing material non-public information and for complying with its disclosure obligations under Regulation FD. A copy of the supplemental investor materials is also furnished as Exhibit 99.2 to this Current Report on Form 8-K and is incorporated herein by reference.
The information in Item 2.02 of this Current Report on Form 8-K and the exhibits attached hereto are intended to be “furnished” and shall not be deemed “filed” for purposes of Section 18 of the Securities Exchange Act of 1934, as amended. Except as shall be expressly set forth by specific reference in such filing, the information contained herein and in the accompanying exhibits shall not be incorporated by reference into any filing with the Securities and Exchange Commission made by the Company, whether made before or after the date hereof, regardless of any general incorporation language in such filing.
| | | | | | | | |
| Item 9.01 | | Financial Statements and Exhibits. |
(d) Exhibits
| | | | | |
| Exhibit No. | Description |
| 99.1 | |
| 99.2 | |
| 104 | Cover Page Interactive Data File (embedded within the Inline XBRL document) |
SIGNATURES
Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned hereunto duly authorized.
| | | | | | | | |
| | |
| | eHealth, Inc. |
| Date: | February 27, 2024 | /s/ John Stelben |
| | John Stelben Chief Financial Officer (Principal Financial Officer) |
eHealth, Inc. Announces Fourth Quarter and Fiscal Year 2023 Results
Fourth quarter revenue growth of 26% YoY driven by strong and profitable Medicare enrollment growth
AUSTIN, Texas — February 27, 2024 — eHealth, Inc. (Nasdaq: EHTH), a leading private online health insurance marketplace, today announced its financial results for the fourth quarter and fiscal year ended December 31, 2023.
| | | | | | | | |
| CEO Comments | | |
| | |
“eHealth’s fourth quarter results reflect the success of our transformation program and company-wide AEP preparedness efforts. We delivered strong Medicare enrollment and revenue growth as well as substantial improvement in our profitability metrics compared to the fourth quarter of last year. Importantly, fourth quarter and full year 2023 operating cash flow exceeded our expectations, reflecting favorable retention trends in our Medicare book of business among other factors. As we return to profitable growth, eHealth has maintained its steadfast commitment to enrollment quality and customer experience, and will continue building a distinct consumer brand as a trusted and unbiased Medicare matchmaker.” – Fran Soistman, Chief Executive Officer |
■Q4 2023 total revenue of $247.7 million increased 26%, including $15.6 million in positive net adjustment revenue, as compared to Q4 2022 total revenue of $196.3 million which includes $11.1 million in positive net adjustment revenue; Q4 2023 total revenue increased 25% year-over-year excluding positive net adjustment revenue.
■Q4 2023 Medicare Advantage approved members were 159,595, an increase of 22% year-over-year.
■Q4 2023 Medicare Advantage LTV increased 11% to $1,151 from $1,033 in Q4 2022, driven primarily by favorable member retention and carrier mix, among other factors.
■Q4 2023 GAAP net income improved $31.5 million year-over-year to $52.2 million compared to Q4 2022 GAAP net income of $20.7 million; Q4 2023 GAAP net income improved $28.2 million year-over-year excluding the impact of positive net adjustment revenue.
■Q4 2023 adjusted EBITDA(1) improved $20.1 million year-over-year to $69.6 million compared to Q4 2022 adjusted EBITDA(1) of $49.5 million; Q4 2023 adjusted EBITDA(1) improved $15.6 million year-over-year excluding the impact of positive net adjustment revenue.
■Operating cash flow of $(6.7) million for the twelve months ended December 31, 2023, outperformed the high-end of our guidance range and represents a significant improvement from operating cash flow of $(26.9) million for the twelve months ended December 31, 2022.
■Cash, cash equivalents and marketable securities of $121.7 million as of December 31, 2023.
■Commissions receivable balance of $918.2 million as of December 31, 2023.
__________
Note: See the tables at the end of this press release for a reconciliation of our GAAP financial measures to our non-GAAP financial measures for the relevant periods and footnote (1) on page 13 at the end of this press release for definitions of our non-GAAP financial measures.
2024 Guidance
Based on information available as of February 27, 2024, we are providing guidance for the full year ending December 31, 2024. These expectations are forward-looking statements and we assume no obligation to update these statements. Actual results may be materially different and are affected by the risk factors and uncertainties identified in this press release and in eHealth’s annual and quarterly reports filed with the Securities and Exchange Commission.
The following guidance is for the full year ending December 31, 2024:
•Total revenue is expected to be in the range of $450 million to $475 million.
•GAAP net income (loss) is expected to be in the range of $(40) million to $(20) million.
•Adjusted EBITDA(1) is expected to be in the range of $(5) million to $20 million.
•Operating cash flow is expected to be in the range of $(15) million to $(5) million.
The above guidance includes the expected impact of positive net adjustment revenue in the range of $0 to $15 million. Excluding the impact of positive net adjustment revenue in both years, the mid-point of our 2024 guidance reflects approximately 12% year-over-year total revenue growth and a substantial improvement in GAAP net income (loss) and adjusted EBITDA(1).
__________
Note: See accompanying footnotes on page 13.
Webcast and Conference Call Information
A webcast and conference call will be held today, Tuesday, February 27, 2024 at 8:30 a.m. Eastern Time / 7:30 a.m. Central Time. Individuals interested in listening to the conference call may do so by dialing (800) 225-9448. The participant passcode is 4737247. The live and archived webcast of the call will also be available under “News and Events” on the Investor Relations page of our website at https://ir.ehealthinsurance.com.
About eHealth, Inc.
We’re Matchmakers. For over 25 years, eHealth has helped millions of Americans find the healthcare coverage that fits their needs at a price they can afford. Consumers can visit our health insurance marketplace at eHealth.com, or call us to speak with a licensed insurance agent at 1-833-964-1202, TTY 711. As a leading independent licensed insurance agency and advisor, eHealth offers access to over 180 health insurers, including national and regional companies.
For more information, visit eHealth.com or follow us on LinkedIn, Facebook, Instagram, and X. Open positions can be found on our career page.
Forward-Looking Statements
This press release contains statements that are forward-looking statements as defined within the Private Securities Litigation Reform Act of 1995. These include statements regarding our expectations regarding our business, operations and strategy, including transformation program, and marketing and growth strategy; our expectations for enrollment growth and quality; our expectations regarding our financial performance and profitability; our expectations regarding our operations and costs, including investment in enrollment growth and business diversification; our estimates regarding total membership, Medicare, individual and family plan, ancillary products and small business memberships; our estimates regarding constrained lifetime values of commissions per approved member by product category; our estimates regarding costs per approved member; our guidance for total revenue, GAAP net income (loss), adjusted EBITDA and operating cash flow; and other statements regarding our future operations, financial condition, prospects and business strategies.
These forward-looking statements are inherently subject to various risks and uncertainties that could cause actual results to differ materially from the statements made. In particular, we are required by Accounting Standards Codification 606 — Revenue from Contracts with Customers to make numerous assumptions that are based on historical trends and our
management’s judgment. These assumptions may change over time and have a material impact on our revenue recognition, guidance, and results of operations. Please review the assumptions stated in this press release carefully.
The risks and uncertainties that could cause our results to differ materially from those expressed or implied by such forward-looking statements include, but are not limited to, our ability to retain existing members and enroll new members during the annual healthcare open enrollment period, the Medicare annual enrollment period, the Medicare Advantage annual open enrollment period and other special enrollment periods; changes in laws, regulations and guidelines, including in connection with healthcare reform or with respect to the marketing and sale of Medicare plans; competition, including competition from government-run health insurance exchanges and other sources; the seasonality of our business and the fluctuation of our operating results; our ability to accurately estimate membership, lifetime value of commissions and commissions receivable; changes in product offerings among carriers on our ecommerce platform and changes in our estimated conversion rate of an approved member to a paying member and the resulting impact of each on our commission revenue; the concentration of our revenue with a small number of health insurance carriers; our ability to execute on our growth strategy and other business initiatives; changes in our management; our ability to hire, train, retain and ensure the productivity of licensed insurance agents, or benefit advisors, and other employees; exposure to security risks and our ability to safeguard the security and privacy of confidential data; our relationships with health insurance carriers; the success of our carrier advertising and sponsorship program; our success in marketing and selling health insurance plans and our unit cost of acquisition; our ability to effectively manage our operations as our business evolves and execute on our transformation plan and other strategic initiatives; the need for health insurance carrier and regulatory approvals in connection with the marketing of Medicare-related insurance products; changes in the market for private health insurance; consumer satisfaction of our service and actions we take to improve the quality of enrollments; changes in member conversion rates; changes in commission rates; our ability to sell qualified health insurance plans to subsidy-eligible individuals and to enroll subsidy-eligible individuals through government-run health insurance exchanges; our ability to derive desired benefits from investments in our business, including membership growth and retention initiatives; our reliance on marketing partners; the success and cost of our marketing efforts, including branding, online advertising, direct-to-consumer mail, email, social media, telephone, television, radio and other marketing efforts; timing of receipt and accuracy of commission reports; payment practices of health insurance carriers; dependence on our operations in China; the restrictions in our debt obligations; the restrictions in our investment agreement with convertible preferred stock investor; our ability to raise additional capital; compliance with insurance, privacy, cybersecurity and other laws and regulations; the outcome of litigation in which we may from time to time be involved; the performance, reliability and availability of our information technology systems, ecommerce platform and underlying network infrastructure, including any new systems we may implement; public health crises, pandemics, natural disasters, changing climate conditions and other extreme events; general economic conditions, including inflation, recession, financial, banking and credit market disruptions; and our ability to affectively administer our self-insurance program. Other factors that could cause operating, financial and other results to differ are described in our most recent Quarterly Report on Form 10-Q or Annual Report on Form 10-K filed with the Securities and Exchange Commission and available on the Investor Relations page of our website at https://ir.ehealthinsurance.com and on the Securities and Exchange Commission’s website at www.sec.gov.
All forward-looking statements in this press release are based on information available to us as of the date hereof, and we do not assume any obligation to update the forward-looking statements provided to reflect events that occur or circumstances that exist after the date on which they were made, except as required by law.
Investor Relations Contact
Kate Sidorovich, CFA
Senior Vice President, Investor Relations & Strategy
investors@ehealth.com
https://ir.ehealthinsurance.com
EHEALTH, INC.
CONDENSED CONSOLIDATED BALANCE SHEETS
(in thousands, unaudited)
| | | | | | | | | | | |
| December 31, 2023 | | December 31, 2022 |
| Assets | | | |
| Current assets: | | | |
| Cash and cash equivalents | $ | 115,722 | | | $ | 144,401 | |
| Short-term marketable securities | 5,930 | | | — | |
| Accounts receivable | 3,993 | | | 2,633 | |
| Contract assets – commissions receivable – current | 244,663 | | | 242,749 | |
| Prepaid expenses and other current assets | 12,044 | | | 11,301 | |
| Total current assets | 382,352 | | | 401,084 | |
| Contract assets – commissions receivable – non-current | 673,514 | | | 641,555 | |
| Property and equipment, net | 4,864 | | | 5,501 | |
| | | |
| Operating lease right-of-use assets | 22,767 | | | 26,516 | |
| Restricted cash | 3,090 | | | 3,239 | |
| Other assets | 26,758 | | | 34,716 | |
| | | |
| | | |
| Total assets | $ | 1,113,345 | | | $ | 1,112,611 | |
| | | |
| Liabilities, convertible preferred stock and stockholders’ equity | | | |
| Current liabilities: | | | |
| Accounts payable | $ | 7,197 | | | $ | 6,732 | |
| Accrued compensation and benefits | 40,800 | | | 20,690 | |
| Accrued marketing expenses | 20,340 | | | 23,770 | |
| | | |
| Lease liabilities – current | 7,070 | | | 6,486 | |
| | | |
| Other current liabilities | 3,131 | | | 2,887 | |
| Total current liabilities | 78,538 | | | 60,565 | |
| Long-term debt | 67,754 | | | 66,129 | |
| | | |
| Deferred income taxes – non-current | 29,687 | | | 32,359 | |
| Lease liabilities – non-current | 28,333 | | | 34,187 | |
| Other non-current liabilities | 4,949 | | | 5,132 | |
| Total liabilities | 209,261 | | | 198,372 | |
| Convertible preferred stock | 298,053 | | | 263,284 | |
| Stockholders’ equity: | | | |
| | | |
| Common stock | 41 | | | 40 | |
| Additional paid-in capital | 798,786 | | | 777,187 | |
| Treasury stock, at cost | (199,998) | | | (199,998) | |
| Retained earnings | 7,284 | | | 73,799 | |
| Accumulated other comprehensive loss | (82) | | | (73) | |
| Total stockholders’ equity | 606,031 | | | 650,955 | |
| Total liabilities, convertible preferred stock and stockholders’ equity | $ | 1,113,345 | | | $ | 1,112,611 | |
EHEALTH, INC.
CONDENSED CONSOLIDATED STATEMENTS OF OPERATIONS
(in thousands, except per share amounts, unaudited)
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
December 31, | | % Change | | Year Ended
December 31, | | % Change |
| 2023 | | 2022 | | | | 2023 | | 2022 | | |
| Revenue: | | | | | | | | | | | |
| Commission | $ | 218,496 | | $ | 170,584 | | 28 | % | | $ | 403,924 | | $ | 361,246 | | 12 | % |
| Other | 29,166 | | 25,737 | | 13 | % | | 48,947 | | 44,110 | | 11 | % |
| Total revenue | 247,662 | | 196,321 | | 26 | % | | 452,871 | | 405,356 | | 12 | % |
Operating costs and expenses(a): | | | | | | | | | | | |
| Cost of revenue | 1,109 | | 857 | | 29 | % | | 1,771 | | 1,647 | | 8 | % |
| Marketing and advertising | 88,155 | | 76,115 | | 16 | % | | 173,326 | | 195,088 | | (11) | % |
| Customer care and enrollment | 58,559 | | 40,388 | | 45 | % | | 159,060 | | 141,099 | | 13 | % |
| Technology and content | 17,155 | | 21,967 | | (22) | % | | 61,027 | | 78,809 | | (23) | % |
| General and administrative | 23,316 | | 17,325 | | 35 | % | | 86,761 | | 71,810 | | 21 | % |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Impairment, restructuring and other charges | — | | 8,926 | | (100) | % | | — | | 19,616 | | (100) | % |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Total operating costs and expenses | 188,294 | | 165,578 | | 14 | % | | 481,945 | | 508,069 | | (5) | % |
| Income (loss) from operations | 59,368 | | 30,743 | | 93 | % | | (29,074) | | (102,713) | | 72 | % |
| Interest expense | (2,852) | | (2,382) | | (20) | % | | (10,974) | | (7,627) | | (44) | % |
| Other income, net | 1,953 | | 1,541 | | 27 | % | | 9,453 | | 3,951 | | 139 | % |
| Income (loss) before income taxes | 58,469 | | 29,902 | | 96 | % | | (30,595) | | (106,389) | | 71 | % |
| Provision for (benefit from) income taxes | 6,279 | | 9,231 | | | | (2,381) | | (17,667) | | |
| Net income (loss) | 52,190 | | 20,671 | | 152 | % | | (28,214) | | (88,722) | | 68 | % |
| Preferred stock dividends | (5,321) | | (4,937) | | | | (20,965) | | (19,357) | | |
| Change in preferred stock redemption value | (5,178) | | (3,162) | | | | (17,336) | | (11,335) | | |
| | | | | | | | | | | |
| Net income (loss) attributable to common stockholders | $ | 41,691 | | $ | 12,572 | | 232 | % | | $ | (66,515) | | $ | (119,414) | | 44 | % |
| | | | | | | | | | | |
Net income (loss) per share attributable to common stockholders(8): | | | | | | | | | | | |
Basic | $ | 1.31 | | $ | 0.41 | | 220 | % | | $ | (2.37) | | $ | (4.36) | | 46 | % |
| Diluted | $ | 1.27 | | $ | 0.41 | | 210 | % | | $ | (2.37) | | $ | (4.36) | | 46 | % |
| Weighted-average number of shares used in per share: | | | | | | | | | | | |
| Basic | 28,469 | | 27,514 | | 3 | % | | 28,016 | | 27,359 | | 2 | % |
| Diluted | 29,370 | | 27,558 | | 7 | % | | 28,016 | | 27,359 | | 2 | % |
| | | | | | | | | | | |
_____________________________ (a) Includes stock-based compensation expense as follows: |
| Marketing and advertising | $ | 603 | | $ | 590 | | | | $ | 2,201 | | $ | 1,901 | | |
| Customer care and enrollment | 58 | | 520 | | | | 2,287 | | 2,096 | | |
| Technology and content | 1,114 | | 1,003 | | | | 4,498 | | 6,015 | | |
| General and administrative | 3,697 | | 2,269 | | | | 14,227 | | 10,304 | | |
| | | | | | | | | | | |
| Total stock-based compensation expense | $ | 5,472 | | $ | 4,382 | | 25 | % | | $ | 23,213 | | $ | 20,316 | | 14 | % |
| | | | | | | | | | | |
Non-GAAP Results(1): | | | | | | | | | | | |
| Adjusted EBITDA | $ | 69,615 | | $ | 49,474 | | 41 | % | | $ | 14,055 | | $ | (41,673) | | 134 | % |
| Adjusted EBITDA margin | 28 | % | | 25 | % | | 12 | % | | 3 | % | | (10) | % | | 130 | % |
__________
Note: See accompanying footnotes on page 13.
EHEALTH, INC.
CONDENSED CONSOLIDATED STATEMENTS OF CASH FLOWS
(in thousands, unaudited)
| | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
December 31, | | Year Ended
December 31, | | |
| | 2023 | | 2022 | | 2023 | | 2022 | | | | |
| Operating activities: | | | | | | | | | | | |
| Net income (loss) | $ | 52,190 | | | $ | 20,671 | | | $ | (28,214) | | | $ | (88,722) | | | | | |
| Adjustments to reconcile net income (loss) to net cash used in operating activities: | | | | | | | | | | | |
| Depreciation and amortization | 632 | | | 874 | | | 2,540 | | | 3,845 | | | | | |
| Amortization of internally developed software | 4,143 | | | 4,549 | | | 17,376 | | | 17,263 | | | | | |
| | | | | | | | | | | |
| Stock-based compensation expense | 5,472 | | | 4,382 | | | 23,213 | | | 20,316 | | | | | |
| Deferred income taxes | 6,639 | | | 8,771 | | | (2,672) | | | (18,436) | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Impairment charges | — | | | 8,368 | | | — | | | 12,102 | | | | | |
| Other non-cash items | 696 | | | 751 | | | 701 | | | 2,084 | | | | | |
| Changes in operating assets and liabilities: | | | | | | | | | | | |
| Accounts receivable | (3,471) | | | (828) | | | (1,361) | | | 3,118 | | | | | |
| Contract assets – commissions receivable | (137,754) | | | (98,650) | | | (33,594) | | | 23,760 | | | | | |
| Prepaid expenses and other assets | 10,649 | | | 10,745 | | | (1,948) | | | 13,473 | | | | | |
| Accounts payable | 306 | | | 89 | | | 487 | | | (7,029) | | | | | |
| Accrued compensation and benefits | 14,008 | | | 5,577 | | | 20,110 | | | 4,232 | | | | | |
| Accrued marketing expenses | 12,917 | | | 15,561 | | | (3,430) | | | (12,614) | | | | | |
| Deferred revenue | (45) | | | 459 | | | 1,278 | | | 175 | | | | | |
| | | | | | | | | | | |
| Accrued expenses and other liabilities | 232 | | | 102 | | | (1,178) | | | (436) | | | | | |
| Net cash used in operating activities | (33,386) | | | (18,579) | | | (6,692) | | | (26,869) | | | | | |
| Investing activities: | | | | | | | | | | | |
| Capitalized internal-use software and website development costs | (1,665) | | | (2,752) | | | (8,693) | | | (15,292) | | | | | |
| Purchases of property and equipment and other assets | (327) | | | (22) | | | (2,086) | | | (214) | | | | | |
| Purchases of marketable securities | (5,912) | | | — | | | (54,514) | | | (8,402) | | | | | |
| Proceeds from redemption and maturities of marketable securities | 8,500 | | | 4,500 | | | 49,400 | | | 49,769 | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Net cash provided by (used in) investing activities | 596 | | | 1,726 | | | (15,893) | | | 25,861 | | | | | |
| Financing activities: | | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Net proceeds from debt financing | — | | | — | | | — | | | 64,862 | | | | | |
| Net proceeds from exercise of common stock options and employee stock purchases | 415 | | | 1,160 | | | 677 | | | 2,214 | | | | | |
| Repurchase of shares to satisfy employee tax withholding obligations | (1,395) | | | (201) | | | (3,330) | | | (3,102) | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Principal payments in connection with leases | (5) | | | (46) | | | (38) | | | (136) | | | | | |
| Payments of preferred stock dividends | (2,660) | | | — | | | (3,533) | | | — | | | | | |
| Net cash provided by (used in) financing activities | (3,645) | | | 913 | | | (6,224) | | | 63,838 | | | | | |
| Effect of exchange rate changes on cash, cash equivalents and restricted cash | 39 | | | 83 | | | (19) | | | (355) | | | | | |
Net increase (decrease) in cash, cash equivalents and restricted cash | (36,396) | | | (15,857) | | | (28,828) | | | 62,475 | | | | | |
| Cash, cash equivalents and restricted cash at beginning of period | 155,208 | | | 163,497 | | | 147,640 | | | 85,165 | | | | | |
| Cash, cash equivalents and restricted cash at end of period | $ | 118,812 | | | $ | 147,640 | | | $ | 118,812 | | | $ | 147,640 | | | | | |
EHEALTH, INC.
SEGMENT INFORMATION
(in thousands, unaudited)
We evaluate our business performance and manage our operations as two distinct reporting segments: Medicare and Employer and Individual (“E&I”). In the fourth quarter of 2023, the Individual, Family and Small Business segment was renamed “Employer and Individual”. The E&I segment name change was to the name only and had no impact on our historical financial position, results of operations, cash flow or segment level results previously reported. This identification of reportable segments is consistent with how the segments report to and are managed by our chief executive officer, who is our chief operating decision maker. The Medicare segment consists primarily of amounts earned from our sale of Medicare-related health insurance plans, including Medicare Advantage, Medicare Supplement and Medicare Part D prescription drug plans (collectively, the “Medicare Plans”), fees earned for the performance of administrative services, amounts earned from our non-broker of record arrangements, our performance of various post-enrollment services for members and to a lesser extent, amounts earned from our sale of ancillary products sold to our Medicare-eligible customers, including but not limited to, dental and vision plans, as well as amounts we are paid in connection with our advertising program for marketing and other services. The E&I segment consists primarily of amounts earned from our sale of individual, family and small business health insurance plans, including both qualified and non-qualified plans, and ancillary products sold to our non-Medicare-eligible customers, including but not limited to, dental, vision, and short-term insurance. To a lesser extent, the E&I segment consists of amounts earned from our online sponsorship and advertising program that allows carriers to purchase advertising space in specific markets in a sponsorship area on our website and our technology licensing and lead referral activities.
Marketing and advertising, customer care and enrollment, technology and content and general and administrative operating expenses that are directly attributable to a segment are reported within the applicable segment. Indirect marketing and advertising, customer care and enrollment and technology and content operating expenses are allocated to each segment based on usage. Corporate consists of other indirect general and administrative operating expenses, excluding stock-based compensation expense, depreciation and amortization, which are managed in a corporate shared services environment and, since they are not the responsibility of segment operating management, are not allocated to the reportable segments and are instead reported within Corporate.
The performance of each reportable segment is evaluated based on several factors, including revenue and segment profit (loss), which is calculated as total revenue for the applicable segment less direct and indirect allocated marketing and advertising, customer care and enrollment, technology and content and general and administrative operating expenses, excluding stock-based compensation expense, depreciation and amortization, impairment, restructuring and other charges, interest expense and other income (expense), net. Senior management uses segment profit (loss) to evaluate segment performance because they believe this measure is indicative of performance trends and the overall earnings potential of each segment.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
December 31, | | % Change | | Year Ended
December 31, | | % Change |
| | 2023 | | 2022 | | | 2023 | | 2022 | |
| Revenue: | | | | | | | | | | | |
| Medicare | $ | 233,680 | | | $ | 180,421 | | | 30 | % | | $ | 406,467 | | | $ | 361,687 | | | 12 | % |
Employer and Individual | 13,982 | | | 15,900 | | | (12) | % | | 46,404 | | | 43,669 | | | 6 | % |
| Total revenue | $ | 247,662 | | | $ | 196,321 | | | 26 | % | | $ | 452,871 | | | $ | 405,356 | | | 12 | % |
| | | | | | | | | | | |
| Segment profit (loss): | | | | | | | | | | | |
| Medicare | $ | 80,287 | | | $ | 53,177 | | | 51 | % | | $ | 54,748 | | | $ | (9,873) | | | 655 | % |
Employer and Individual | 7,104 | | | 9,153 | | | (22) | % | | 25,841 | | | 21,438 | | | 21 | % |
Segment profit | 87,391 | | | 62,330 | | | 40 | % | | 80,589 | | | 11,565 | | | 597 | % |
| Corporate | (17,776) | | | (12,856) | | | | | (66,534) | | | (53,238) | | | |
| Stock-based compensation expense | (5,472) | | | (4,382) | | | | | (23,213) | | | (20,316) | | | |
| | | | | | | | | | | |
| Depreciation and amortization | (4,775) | | | (5,423) | | | | | (19,916) | | | (21,108) | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Impairment, restructuring and other charges | — | | | (8,926) | | | | | — | | | (19,616) | | | |
| Interest expense | (2,852) | | | (2,382) | | | | | (10,974) | | | (7,627) | | | |
| Other income, net | 1,953 | | | 1,541 | | | | | 9,453 | | | 3,951 | | | |
Income (loss) before income taxes | $ | 58,469 | | | $ | 29,902 | | | 96 | % | | $ | (30,595) | | | $ | (106,389) | | | 71 | % |
EHEALTH, INC.
COMMISSION REVENUE
(in thousands, unaudited)
Our commission revenue results from approval of an application from health insurance carriers, which we define as our customers under Accounting Standards Codification 606 — Revenue from Contracts with Customers (“ASC 606”). Our commission revenue is primarily comprised of commissions from health insurance carriers which is computed using the estimated constrained lifetime values as the “constrained LTVs” of commission payments that we expect to receive. Our commissions may include certain bonus payments, which are generally based on our attaining predetermined target sales levels or other objectives, as determined by the health insurance carriers. For Medicare Advantage and Medicare Part D prescription drug plans, our commissions also include regular payments related to administrative services we perform.
The following table presents commission revenue by product for the periods indicated:
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
December 31, | | % Change | | Year Ended
December 31, | | % Change |
| 2023 | | 2022 | | | 2023 | | 2022 | |
| Medicare | | | | | | | | | | | |
| Medicare Advantage | $ | 192,618 | | | $ | 141,501 | | | 36 | % | | $ | 335,849 | | | $ | 293,562 | | | 14 | % |
| Medicare Supplement | 6,039 | | | 6,128 | | | (1) | % | | 13,825 | | | 17,419 | | | (21) | % |
| Medicare Part D | 6,494 | | | 5,006 | | | 30 | % | | 11,180 | | | 7,171 | | | 56 | % |
| Total Medicare | 205,151 | | | 152,635 | | | 34 | % | | 360,854 | | | 318,152 | | | 13 | % |
Individual and Family | | | | | | | | | | | |
| Non-Qualified Health Plans | 3,736 | | | 6,460 | | | (42) | % | | 10,640 | | | 12,430 | | | (14) | % |
| Qualified Health Plans | 1,936 | | | 2,460 | | | (21) | % | | 6,020 | | | 5,435 | | | 11 | % |
Total Individual and Family | 5,672 | | | 8,920 | | | (36) | % | | 16,660 | | | 17,865 | | | (7) | % |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Ancillary | 3,251 | | | 3,386 | | | (4) | % | | 10,754 | | | 11,466 | | | (6) | % |
| Small Business | 5,112 | | | 3,296 | | | 55 | % | | 17,669 | | | 11,842 | | | 49 | % |
| Commission Bonus and Other | (690) | | | 2,347 | | | (129) | % | | (2,013) | | | 1,921 | | | (205) | % |
| Total Commission Revenue | $ | 218,496 | | | $ | 170,584 | | | 28 | % | | $ | 403,924 | | | $ | 361,246 | | | 12 | % |
The following table presents a summary of commission revenue by segment for the periods indicated:
| | | | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
December 31, | | Year Ended
December 31, | | |
| | 2023 | | 2022 | | 2023 | | 2022 | |
| Medicare | | | | | | | | | |
| Commission Revenue from Members Approved During the Period | $ | 194,295 | | | $ | 148,716 | | | $ | 326,087 | | | $ | 322,506 | | | |
Net Commission Revenue from Members Approved in Prior Periods(a) | 10,798 | | | 6,726 | | | 33,544 | | | (2,326) | | | |
| Total Medicare Segment Commission Revenue | 205,093 | | | 155,442 | | | 359,631 | | | 320,180 | | | |
Employer and Individual | | | | | | | | | |
| Commission Revenue from Members Approved During the Period | 5,954 | | | 8,104 | | | 19,789 | | | 22,358 | | | |
| Commission Revenue from Renewals of Small Business Members During the Period | 2,674 | | | 2,700 | | | 9,973 | | | 9,981 | | | |
Net Commission Revenue from Members Approved in Prior Periods(a) | 4,775 | | | 4,338 | | | 14,531 | | | 8,727 | | | |
Total Employer and Individual Segment Commission Revenue | 13,403 | | | 15,142 | | | 44,293 | | | 41,066 | | | |
| Total Commission Revenue | $ | 218,496 | | | $ | 170,584 | | | $ | 403,924 | | | $ | 361,246 | | | |
_____________
(a) These amounts reflect our revised estimates of cash collections for certain members approved prior to the relevant reporting period that are recognized as adjustments to revenue within the relevant reporting period. The net adjustment revenue includes both increases in revenue for certain prior period cohorts as well as reductions in revenue for certain prior period cohorts. The total reductions to revenue from members approved in prior periods were $0.6 million and $0.7 million for the three months ended December 31, 2023 and 2022, respectively, and $4.3 million and $16.5 million for the year ended December 31, 2023 and 2022, respectively. These reductions to revenue primarily relate to the Medicare segment.
EHEALTH, INC.
SUMMARY OF SELECTED METRICS
(in thousands, except member and per member data, unaudited)
Selected Metrics — Fourth Quarter of 2023
| | | | | | | | | | | | | | | | | |
| Three Months Ended
December 31, | | % Change |
| 2023 | | 2022 | |
Approved Members(2) | | | | | |
| Medicare | | | | | |
| Medicare Advantage | 159,595 | | 131,235 | | 22 | % |
| Medicare Supplement | 6,868 | | 6,340 | | 8 | % |
| Medicare Part D | 20,104 | | 23,894 | | (16) | % |
| Total Medicare | 186,567 | | 161,469 | | 16 | % |
| Individual and Family | 9,207 | | 14,010 | | (34) | % |
| Ancillary | 14,205 | | 17,749 | | (20) | % |
| Small Business | 2,406 | | 2,947 | | (18) | % |
| Total Approved Members | 212,385 | | 196,175 | | 8 | % |
| | | | | |
Constrained Lifetime Value of Commissions per Approved Member(3) | | | | | |
Medicare(a) | | | | | |
| Medicare Advantage | $ | 1,151 | | $ | 1,033 | | 11 | % |
| Medicare Supplement | 931 | | 945 | | (1) | % |
| Medicare Part D | 220 | | 182 | | 21 | % |
| Individual and Family | | | | | |
| Non-Qualified Health Plans | 400 | | 404 | | (1) | % |
| Qualified Health Plans | 378 | | 382 | | (1) | % |
| Ancillary | | | | | |
| Short-term | 172 | | 170 | | 1 | % |
| Dental | 117 | | 117 | | — | % |
| Vision | 83 | | 69 | | 20 | % |
| Small Business | 231 | | 227 | | 2 | % |
(a) Constraints for all Medicare products remained the same for the periods presented. | | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
Expense Metrics per Approved Member(4) | | | | | |
| Medicare | | | | | |
Customer care and enrollment cost per Medicare Advantage (“MA”)-equivalent approved member | $ | 323 | | $ | 259 | | 25 | % |
| Variable marketing cost per MA-equivalent approved member | 456 | | 470 | | (3) | % |
| Total acquisition cost per MA-equivalent approved member | $ | 779 | | $ | 729 | | 7 | % |
Individual and Family Plan (“IFP”) | | | | | |
| Customer care and enrollment cost per IFP-equivalent approved member | $ | 194 | | $ | 137 | | 42 | % |
| Variable marketing cost per IFP-equivalent approved member | 84 | | 68 | | 24 | % |
| Total acquisition cost per IFP-equivalent approved member | $ | 278 | | $ | 205 | | 36 | % |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
__________Note: See accompanying footnotes on page 13.
EHEALTH, INC.
SUMMARY OF SELECTED METRICS
(in thousands, except member and per member data, unaudited)
Selected Metrics — Year Ended December 31, 2023
| | | | | | | | | | | | | | | | | |
| Year Ended
December 31, | | % Change |
| 2023 | | 2022 | |
Approved Members(2) | | | | | |
| Medicare | | | | | |
| Medicare Advantage | 290,712 | | | 302,949 | | | (4) | % |
| Medicare Supplement | 17,386 | | | 18,569 | | | (6) | % |
| Medicare Part D | 29,378 | | | 40,094 | | | (27) | % |
| Total Medicare | 337,476 | | | 361,612 | | | (7) | % |
| Individual and Family | 27,318 | | | 33,271 | | | (18) | % |
| | | | | |
| | | | | |
| | | | | |
| Ancillary | 56,789 | | | 72,004 | | | (21) | % |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| Small Business | 7,613 | | | 9,722 | | | (22) | % |
| Total Approved Members | 429,196 | | | 476,609 | | | (10) | % |
| | | | | | | | | | | | | | | | | |
| As of December 31, | | % Change |
| 2023 | | 2022 | |
Estimated Membership(5) | | | | | |
Medicare(6) | | | | | |
| Medicare Advantage | 622,896 | | | 645,864 | | | (4) | % |
| Medicare Supplement | 110,826 | | | 100,039 | | | 11 | % |
| Medicare Part D | 210,876 | | | 229,962 | | | (8) | % |
| Total Medicare | 944,598 | | | 975,865 | | | (3) | % |
| | | | | |
| | | | | |
| | | | | |
Individual and Family(6) | 86,452 | | | 102,971 | | | (16) | % |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
Ancillary(6) | 180,741 | | | 214,570 | | | (16) | % |
Small Business(7) | 46,225 | | | 45,584 | | | 1 | % |
| Total Estimated Membership | 1,258,016 | | | 1,338,990 | | | (6) | % |
__________
Note: See accompanying footnotes on page 13.
EHEALTH, INC.
RECONCILIATION OF GAAP TO NON-GAAP FINANCIAL MEASURES
(unaudited)
Reconciliation of GAAP Operating Costs and Expenses to Non-GAAP Operating Costs and Expenses(1) (in thousands):
| | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
December 31, | | Year Ended
December 31, |
| 2023 | | 2022 | | 2023 | | 2022 |
| GAAP marketing and advertising expense | $ | 88,155 | | | $ | 76,115 | | | $ | 173,326 | | | $ | 195,088 | |
Stock-based compensation expense | (603) | | | (590) | | | (2,201) | | | (1,901) | |
Non-GAAP marketing and advertising expense(1) | $ | 87,552 | | | $ | 75,525 | | | $ | 171,125 | | | $ | 193,187 | |
| | | | | | | |
| GAAP customer care and enrollment expense | $ | 58,559 | | | $ | 40,388 | | | $ | 159,060 | | | $ | 141,099 | |
| Stock-based compensation expense | (58) | | | (520) | | | (2,287) | | | (2,096) | |
Non-GAAP customer care and enrollment expense(1) | $ | 58,501 | | | $ | 39,868 | | | $ | 156,773 | | | $ | 139,003 | |
| | | | | | | |
| GAAP technology and content expense | $ | 17,155 | | | $ | 21,967 | | | $ | 61,027 | | | $ | 78,809 | |
| Stock-based compensation expense | (1,114) | | | (1,003) | | | (4,498) | | | (6,015) | |
Non-GAAP technology and content expense(1) | $ | 16,041 | | | $ | 20,964 | | | $ | 56,529 | | | $ | 72,794 | |
| | | | | | | |
| GAAP general and administrative expense | $ | 23,316 | | | $ | 17,325 | | | $ | 86,761 | | | $ | 71,810 | |
| Stock-based compensation expense | (3,697) | | | (2,269) | | | (14,227) | | | (10,304) | |
Non-GAAP general and administrative expense(1) | $ | 19,619 | | | $ | 15,056 | | | $ | 72,534 | | | $ | 61,506 | |
| | | | | | | |
| GAAP operating costs and expenses | $ | 188,294 | | | $ | 165,578 | | | $ | 481,945 | | | $ | 508,069 | |
| Stock-based compensation expense | (5,472) | | | (4,382) | | | (23,213) | | | (20,316) | |
| | | | | | | |
| | | | | | | |
| Impairment, restructuring and other charges | — | | | (8,926) | | | — | | | (19,616) | |
| | | | | | | |
Non-GAAP operating costs and expenses(1) | $ | 182,822 | | | $ | 152,270 | | | $ | 458,732 | | | $ | 468,137 | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
Reconciliation of GAAP Net Income (Loss) Attributable to Common Stockholders to Adjusted EBITDA(1) and Adjusted EBITDA Margin(1) (in thousands):
| | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
December 31, | | Year Ended
December 31, |
| 2023 | | 2022 | | 2023 | | 2022 |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
GAAP net income (loss) attributable to common stockholders | $ | 41,691 | | $ | 12,572 | | $ | (66,515) | | $ | (119,414) |
| Preferred stock dividends | 5,321 | | 4,937 | | 20,965 | | 19,357 |
| Change in preferred stock redemption value | 5,178 | | 3,162 | | 17,336 | | 11,335 |
| GAAP net income (loss) | 52,190 | | 20,671 | | (28,214) | | (88,722) |
| Stock-based compensation expense | 5,472 | | 4,382 | | 23,213 | | 20,316 |
| | | | | | | |
| Depreciation and amortization | 4,775 | | 5,423 | | 19,916 | | 21,108 |
| | | | | | | |
| Impairment, restructuring and other charges | — | | 8,926 | | — | | 19,616 |
| | | | | | | |
| Interest expense | 2,852 | | 2,382 | | 10,974 | | 7,627 |
| Other income, net | (1,953) | | (1,541) | | (9,453) | | (3,951) |
Provision for (benefit from) income taxes | 6,279 | | 9,231 | | (2,381) | | (17,667) |
| Adjusted EBITDA | $ | 69,615 | | $ | 49,474 | | $ | 14,055 | | $ | (41,673) |
Net income (loss) margin | 21 | % | | 11 | % | | (6) | % | | (22) | % |
| Adjusted EBITDA margin | 28 | % | | 25 | % | | 3 | % | | (10) | % |
__________
Note: See accompanying footnotes on page 13.
EHEALTH, INC.
RECONCILIATION OF GAAP TO NON-GAAP FINANCIAL MEASURES
(unaudited)
Reconciliation of Guidance GAAP Net Loss Attributable to Common Stockholders to Adjusted EBITDA(1) (in millions):
| | | | | | | | | | | |
| Full Year 2024 Guidance |
| Low | | High |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| GAAP net loss attributable to common stockholders | $ | (85.0) | | | $ | (65.0) | |
| Impact from preferred stock | 45.0 | | | 45.0 | |
| GAAP net income (loss) | (40.0) | | | (20.0) | |
| Stock-based compensation expense | 20.0 | | | 17.0 | |
| Depreciation and amortization | 19.0 | | | 18.0 | |
| Impairment, restructuring and other charges | 1.0 | | | 1.0 | |
| | | |
Interest expense | 11.0 | | | 10.0 | |
| Other expense, net | (8.0) | | | (9.0) | |
| Benefit from income taxes | (8.0) | | | 3.0 | |
| Adjusted EBITDA | $ | (5.0) | | | $ | 20.0 | |
__________
Note: See accompanying footnotes on page 13.
EHEALTH, INC.
Footnotes to Preceding Financial Statements and Metrics
(1)Non-GAAP Financial Information
This press release includes financial measures that are not calculated in accordance with U.S. generally accepted accounting principles (GAAP). To supplement eHealth’s condensed consolidated financial statements presented in accordance with GAAP, eHealth presents investors with non-GAAP financial measures, including non-GAAP operating costs and expenses, adjusted EBITDA and adjusted EBITDA margin.
•Non-GAAP operating costs and expenses are calculated by excluding the effect of expensing stock-based compensation related to stock options, restricted stock awards, performance-based and market-based awards and employee stock purchase plan. Total non-GAAP operating costs and expenses is calculated by excluding the effect of expensing stock-based compensation related to stock options, restricted stock awards, performance-based and market-based awards and employee stock purchase plan and impairment, restructuring and other charges.
•Adjusted EBITDA is calculated by excluding dividends for preferred stock and change in preferred stock redemption value (together the “impact from preferred stock”), provision for (benefit from) income taxes, depreciation and amortization, stock-based compensation expense, impairment, restructuring and other charges, interest expense, other income (expense), net, and other non-recurring charges from GAAP net income (loss) attributable to common stockholders. Other non-recurring charges to GAAP net income (loss) attributable to common stockholders may include transaction expenses in connection with capital raising transactions (whether debt, equity or equity-linked) and acquisitions, whether or not consummated, purchase price adjustments and the cumulative effect of a change in accounting principles.
•Adjusted EBITDA margin is calculated as adjusted EBITDA divided by revenue.
eHealth believes that the presentation of these non-GAAP financial measures provides important supplemental information to management and investors regarding financial and business trends relating to eHealth’s financial condition and results of operations. Management believes that the use of these non-GAAP financial measures provides consistency and comparability with eHealth’s past financial reports. Management also believes that the items described above provide an additional measure of eHealth’s operating results and facilitates comparisons of eHealth’s core operating performance against prior periods and business model objectives. This information is provided to investors in order to facilitate additional analyses of past, present and future operating performance and as a supplemental means to evaluate eHealth’s ongoing operations. eHealth believes that these non-GAAP financial measures are useful to investors in their assessment of eHealth’s operating performance.
Non-GAAP operating costs and expenses, adjusted EBITDA and adjusted EBITDA margin are not calculated in accordance with GAAP, and should be considered supplemental to, and not as a substitute for, or superior to, financial measures calculated in accordance with GAAP. Non-GAAP financial measures used in this press release have limitations in that they do not reflect all of the revenue and costs associated with the operations of eHealth’s business and do not reflect income tax as determined in accordance with GAAP. As a result, you should not consider these measures in isolation or as a substitute for analysis of eHealth’s results as reported under GAAP. eHealth expects to continue to incur the stock-based compensation costs and depreciation and amortization described above, and exclusion of these costs, and their related income tax benefits, from non-GAAP financial measures should not be construed as an inference that these costs are unusual or infrequent. eHealth compensates for these limitations by prominently disclosing GAAP net income (loss), GAAP net income (loss) attributable to common stockholders and GAAP net income (loss) margin and providing investors with reconciliations from eHealth’s GAAP operating results to the non-GAAP financial measures for the relevant periods.
The tables above provide more details on the GAAP financial measures that are most directly comparable to the non-GAAP financial measures described above and the related reconciliations between these financial measures.
(2)Approved members represent the number of individuals on submitted applications that were approved by the relevant insurance carrier for the identified product during the current period. The applications may be submitted in either the current period or prior periods. Not all approved members ultimately become paying members.
(3)Constrained lifetime value (“LTV”) of commissions per approved member for Medicare, individual and family and ancillary plans represents commissions estimated to be collected over the estimated life of an approved member’s plan after applying constraints in accordance with our revenue recognition policy. Constrained LTV of commissions per approved member for small business represents the estimated commissions we expect to collect from the plan over the following twelve months. The estimate is driven by multiple factors, including but not limited to, contracted commission rates, carrier mix, estimated average plan duration, the regulatory environment, and cancellations of insurance plans offered by health insurance carriers with which we have a relationship and applied constraints. The constraints are applied to help ensure that commissions estimated to be collected over the estimated life of an approved member’s plan are recognized as revenue only to the extent that it is probable that a significant reversal in the amount of cumulative revenue recognized will not occur when the uncertainty associated with future commissions receivable from the plan is subsequently resolved. These factors may result in varying values from period to period.
(4)Expense Metrics per Approved Member: Marketing initiatives are an important component of our strategy to increase revenue and are primarily designed to encourage consumers to complete an application for health insurance. We calculate and evaluate the customer care and enrollment (“CC&E”) expense per approved member and the variable marketing cost per approved member. We incur CC&E expenses in assisting applicants during the enrollment process. Variable marketing costs represent costs incurred in
EHEALTH, INC.
Footnotes to Preceding Financial Statements and Metrics
member acquisition from our direct marketing and marketing partner channels. Variable marketing costs exclude fixed overhead costs, such as personnel related costs, consulting expenses, facilities and other operating costs allocated to the marketing and advertising department.
The numerator used to calculate each member acquisition metric discussed above is the portion of the respective operating expenses for CC&E and marketing and advertising that is directly related to member acquisition for our sale of Medicare Advantage, Medicare Supplement and Medicare Part D prescription drug plans (collectively, the “Medicare Plans”) and for all individual and family major medical plans and short-term health insurance plans (collectively, “IFP Plans”), respectively. The denominator used to calculate each metric is based on a derived metric that represents the relative value of the new members acquired. For Medicare Plans, we call this derived metric Medicare Advantage (“MA”)-equivalent approved members, and for IFP Plans, we call this derived metric IFP-equivalent approved members. MA-equivalent approved members is a derived metric with a Medicare Part D approved member being weighted at 25% of a Medicare Advantage member and a Medicare Supplement member based on their relative LTVs at the time of our adoption of ASC 606. We calculate the number of MA-equivalent approved members by adding the total number of approved Medicare Advantage and Medicare Supplement members and 25% of the total number of approved Medicare Part D members during the periods presented. IFP-equivalent approved members is a derived metric with a short-term approved member being weighted at 33% of a major medical individual and family health insurance plan member based on their relative LTVs at the time of our adoption of ASC 606. We calculate the number of IFP-equivalent approved members by adding the total number of approved qualified and non-qualified health plan members and 33% of the total number of short-term approved members during the period presented.
(5)Estimated membership represents the estimated number of members active as of the date indicated based on the number of members for whom we have received or applied a commission payment during the period of estimation. There is generally up to a few months lag between newly approved plans and the receipt of commission payments from the health insurance carrier. A member who purchases and is active on multiple standalone insurance plans will be counted as a member more than once.
Health insurance carriers bill and collect insurance premiums paid by our members. The carriers do not report to us the number of members that we have as of a given date. The majority of our members who terminate their policies do so by discontinuing their premium payments to the carrier or notifying the carrier directly and do not inform us of the cancellation. Also, some of our members pay their premiums less frequently than monthly. Given the number of months required to observe non-payment of commissions in order to confirm cancellations, we estimate the number of members who are active on insurance policies as of a specified date.
After we have estimated membership for a period, we may receive information from health insurance carriers that would have impacted the estimate if we had received the information prior to the date of estimation. We may receive commission payments or other information that indicates that a member who was not included in our estimates for a prior period was in fact an active member at that time, or that a member who was included in our estimates was in fact not an active member of ours. For instance, we reconcile information carriers provide to us and may determine that we were not historically paid commissions owed to us, which would cause us to have underestimated membership. Conversely, carriers may require us to return commission payments paid in a prior period due to policy cancellations for members we previously estimated as being active. We do not update our estimated membership numbers reported in previous periods. Instead, we reflect updated information regarding our historical membership in the membership estimate for the current period. If we experience a significant variance in historical membership as compared to our initial estimates, while we keep the prior period data consistent with previously reported amounts, we may provide the updated information in other communications or disclosures. As a result of the delay in our receipt of information from insurance carriers, actual trends in our membership are most discernible over periods longer than from one quarter to the next, making it difficult for us to determine with any certainty the impact of current conditions on our membership retention. Various circumstances could cause the assumptions and estimates that we make in connection with estimating our membership to be inaccurate, which would cause our membership estimates to be inaccurate.
(6)To estimate the number of members on Medicare-related, individual and family, and ancillary health insurance plans, we take the respective sum of (i) the number of members for whom we have received or applied a commission payment for a month that may be up to three months prior to the date of estimation (after reducing that number using historical experience for assumed member cancellations over the period being estimated); and (ii) the number of approved members over that period (after reducing that number using historical experience for an assumed number of members who do not accept their approved policy and for estimated member cancellations through the date of the estimate). To the extent we determine through confirmations from a health insurance carrier that a commission payment is delayed or is inaccurate as of the date of estimation, we adjust the estimated membership to also reflect the number of members for whom we expect to receive or to refund a commission payment. Further, to the extent we have received substantially all of the commission payments related to a given month during the period being estimated, we will take the number of members for whom we have received or applied a commission payment during the month of estimation. For ancillary health insurance plans, the one to three-month period varies by insurance product and is largely dependent upon the timeliness of commission payment and related reporting from the related carriers.
(7)To estimate the number of members on small business health insurance plans, we use the number of initial members at the time the group was approved, and we update this number for changes in membership if such changes are reported to us by the group or carrier. However, groups generally notify the carrier directly of policy cancellations and increases or decreases in group size without informing us. Health insurance carriers often do not communicate policy cancellation information or group size changes to us. We often are made aware of policy cancellations and group size changes at the time of annual renewal and update our membership statistics accordingly in the period they are reported.
EHEALTH, INC.
Footnotes to Preceding Financial Statements and Metrics
(8)We apply the two-class method in calculating net income (loss) per share attributable to common stockholders as our Series A convertible preferred stock is considered a participating security, Accordingly, such securities are included in the earnings allocation in calculating income per share. Diluted income (loss) per common share is calculated using the more dilutive of the two-class method or as-converted method. The two-class method uses net income (loss) available to common stockholders and assumes conversion of all potential shares other than participating securities. The as-converted method uses net income (loss) available to common stockholders and assumes conversion of all potential shares including participating securities to the extent they are not anti-dilutive. Net loss attributable to common stockholders is not allocated to the convertible preferred stock as the holder of the Series A preferred stock does not have a contractual obligation to share in losses. For the three months ended December 31, 2023 and 2022, net income allocated to common stockholders (basic) was $37,221 and $11,265, respectively, and net income allocated to participating securities (basic) was $4,469 and $1,307, respectively. For the three months ended December 31, 2023 and 2022, net income allocated to common stockholders (diluted) was $37,344 and $11,267, respectively, and net income allocated to participating securities (diluted) was $4,346 and $1,305, respectively.

©2024 eHealthInsurance Services, Inc. Q4 & FY 2023 Financial Results 1

©2024 eHealthInsurance Services, Inc. 2 Safe Harbor Statement Forward-Looking Statements This presentation includes forward-looking statements within the meaning of the federal securities laws. Forward-looking statements generally relate to future events or our future financial or operating performance. Forward-looking statements in this presentation include, but are not limited to, the following: our estimates regarding Medicare enrollment growth and estimated Medicare membership; our estimates regarding commissions receivable collection and our retention rates; our estimates of constrained lifetime value of commissions per approved member; our 2024 operational priorities, including our local market strategy, branding, and member loyalty and retention strategy; our guidance for total revenue, GAAP net loss, adjusted EBITDA and operating cash flow; our investments in technology and operational initiatives and expected impact of these investments on our business; our expectations regarding our business, industry and market trends, including regulatory proposals, market opportunity, consumer demand and our competitive advantage; and other statements regarding our future operations, financial condition, prospects and business strategies. Our expectations and beliefs regarding these matters may not materialize, and actual results in future periods are subject to risks and uncertainties that could cause actual results to differ materially from those projected. These risks include those set forth in our filings with the Securities and Exchange Commission, including our latest Form 10-Q and 10-K. The forward-looking statements in this presentation are based on information available to us as of today, and we disclaim any obligation to update any forward- looking statements, except as required by law. Non-GAAP Information This presentation includes both GAAP and non-GAAP financial measures. The presentation of non-GAAP financial information is not intended to be considered in isolation or as a substitute for results prepared in accordance with GAAP. A reconciliation of the non-GAAP financial measures included in this presentation to the most directly comparable GAAP financial measures is available in the Appendix to this presentation. Management uses both GAAP and non-GAAP information in evaluating and operating its business internally and as such has determined that it is important to provide this information to investors.
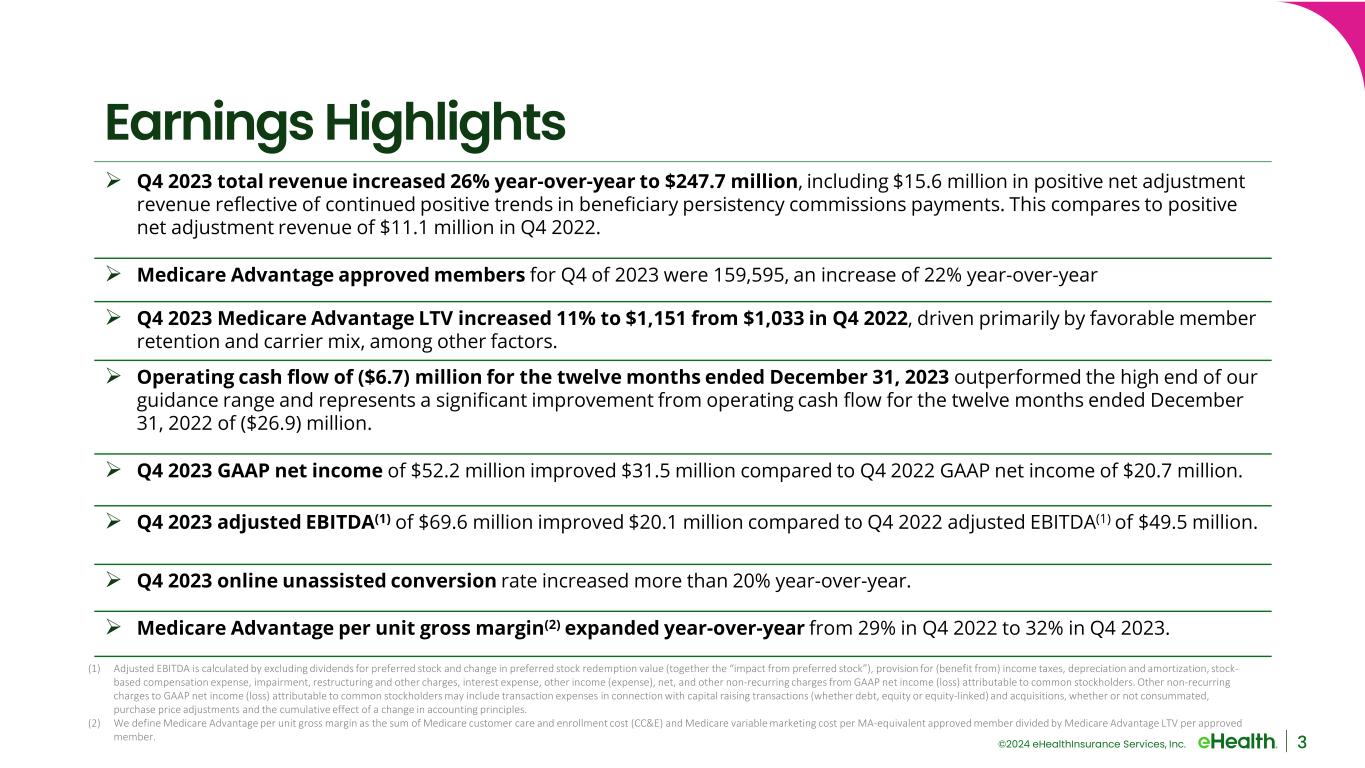
©2024 eHealthInsurance Services, Inc. 3 Earnings Highlights Q4 2023 total revenue increased 26% year-over-year to $247.7 million, including $15.6 million in positive net adjustment revenue reflective of continued positive trends in beneficiary persistency commissions payments. This compares to positive net adjustment revenue of $11.1 million in Q4 2022. Medicare Advantage approved members for Q4 of 2023 were 159,595, an increase of 22% year-over-year Q4 2023 Medicare Advantage LTV increased 11% to $1,151 from $1,033 in Q4 2022, driven primarily by favorable member retention and carrier mix, among other factors. Operating cash flow of ($6.7) million for the twelve months ended December 31, 2023 outperformed the high end of our guidance range and represents a significant improvement from operating cash flow for the twelve months ended December 31, 2022 of ($26.9) million. Q4 2023 GAAP net income of $52.2 million improved $31.5 million compared to Q4 2022 GAAP net income of $20.7 million. Q4 2023 adjusted EBITDA(1) of $69.6 million improved $20.1 million compared to Q4 2022 adjusted EBITDA(1) of $49.5 million. Q4 2023 online unassisted conversion rate increased more than 20% year-over-year. Medicare Advantage per unit gross margin(2) expanded year-over-year from 29% in Q4 2022 to 32% in Q4 2023. (1) Adjusted EBITDA is calculated by excluding dividends for preferred stock and change in preferred stock redemption value (together the “impact from preferred stock”), provision for (benefit from) income taxes, depreciation and amortization, stock- based compensation expense, impairment, restructuring and other charges, interest expense, other income (expense), net, and other non-recurring charges from GAAP net income (loss) attributable to common stockholders. Other non-recurring charges to GAAP net income (loss) attributable to common stockholders may include transaction expenses in connection with capital raising transactions (whether debt, equity or equity-linked) and acquisitions, whether or not consummated, purchase price adjustments and the cumulative effect of a change in accounting principles. (2) We define Medicare Advantage per unit gross margin as the sum of Medicare customer care and enrollment cost (CC&E) and Medicare variable marketing cost per MA-equivalent approved member divided by Medicare Advantage LTV per approved member.
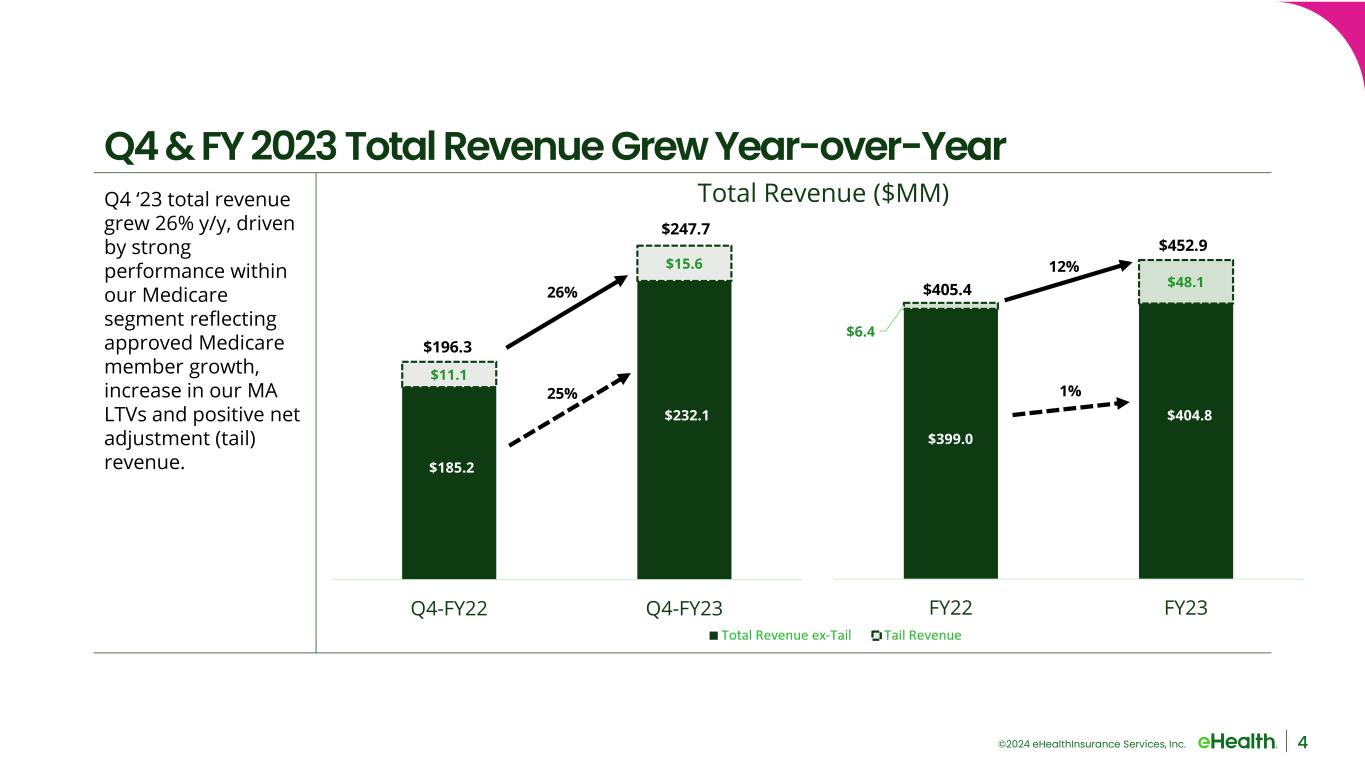
©2024 eHealthInsurance Services, Inc. Q4 ‘23 total revenue grew 26% y/y, driven by strong performance within our Medicare segment reflecting approved Medicare member growth, increase in our MA LTVs and positive net adjustment (tail) revenue. 4 Q4 & FY 2023 Total Revenue Grew Year-over-Year $11.1 $15.6 Q4-FY22 Q4-FY23 26% $196.3 $247.7 $185.2 $232.1 25% $6.4 $48.1 FY22 FY23 $405.4 $452.9 $399.0 $404.8 12% 1% Total Revenue ($MM)
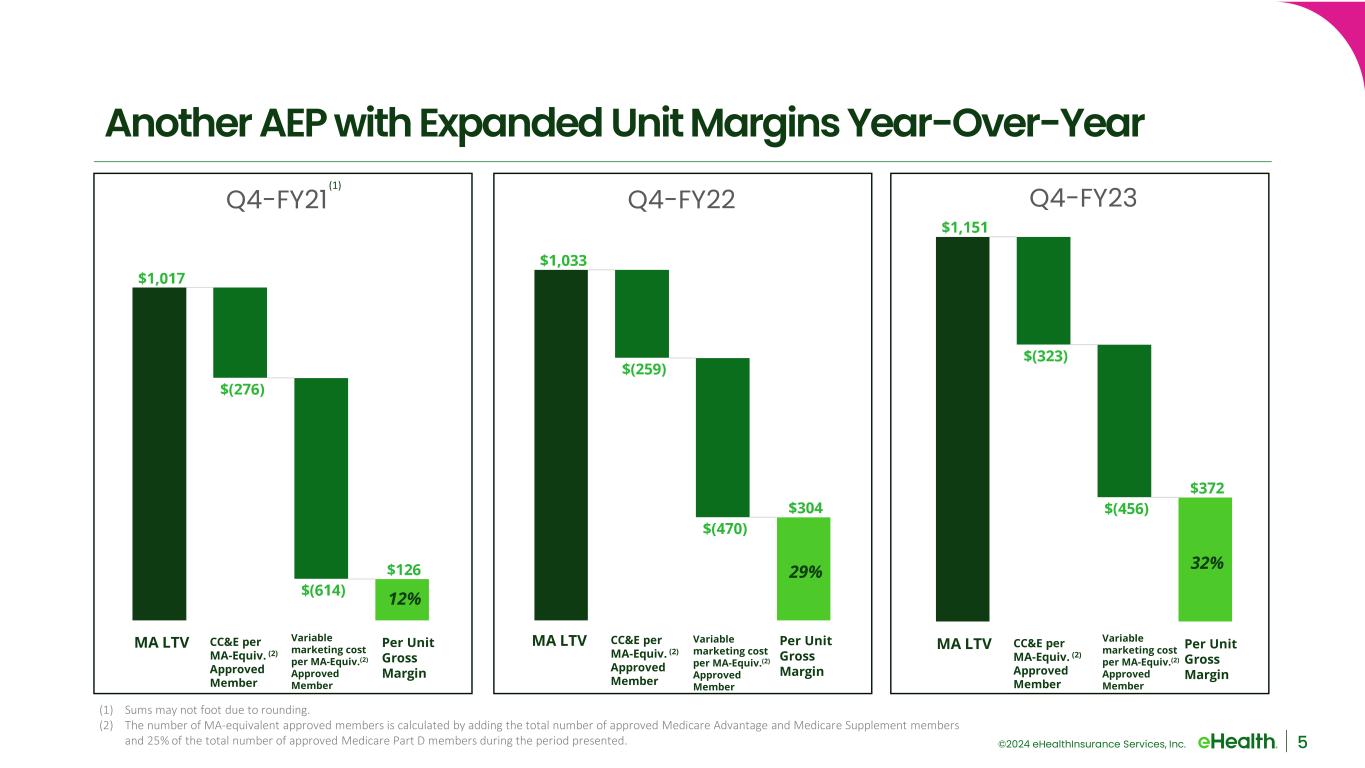
©2024 eHealthInsurance Services, Inc. 5 Another AEP with Expanded Unit Margins Year-Over-Year MA LTV Variable marketing cost per MA-Equiv.(2) Approved Member CC&E per MA-Equiv. (2) Approved Member Per Unit Gross Margin (1) Sums may not foot due to rounding. (2) The number of MA-equivalent approved members is calculated by adding the total number of approved Medicare Advantage and Medicare Supplement members and 25% of the total number of approved Medicare Part D members during the period presented. Q4-FY21 Q4-FY22 Q4-FY23 MA LTV Variable marketing cost per MA-Equiv.(2) Approved Member CC&E per MA-Equiv. (2) Approved Member Per Unit Gross Margin MA LTV Variable marketing cost per MA-Equiv.(2) Approved Member CC&E per MA-Equiv. (2) Approved Member Per Unit Gross Margin 12% 29% 32% (1)

©2024 eHealthInsurance Services, Inc. $49.5 $69.6 Q4-FY22 Q4-FY23 Q4 Adjusted EBITDA ($MM) Q4 & FY 2023 Profitability Improved Year-Over-Year On a year-over-year basis, FY 2023 GAAP Net Income improved $60.5 million, and adjusted EBITDA(1) improved $55.7 million compared to FY 2022. 6 (1) Adjusted EBITDA is calculated by excluding the impact from preferred stock, provision for (benefit from) income taxes, depreciation and amortization, stock-based compensation expense, impairment, restructuring and other charges, interest expense, other income (expense), net, and other non-recurring charges from GAAP net income (loss) attributable to common stockholders. Other non-recurring charges to GAAP net income (loss) attributable to common stockholders may include transaction expenses in connection with capital raising transactions (whether debt, equity or equity-linked) and acquisitions, whether or not consummated, purchase price adjustments and the cumulative effect of a change in accounting principles. (1) ($41.7) $14.1 FY2022 FY2023 FY Adjusted EBITDA ($MM) $20.7 $52.2 Q4-FY22 Q4-FY23 Q4 GAAP Net Income ($MM) ($88.7) ($28.2) FY2022 FY2023 FY GAAP Net Loss ($MM) (1)
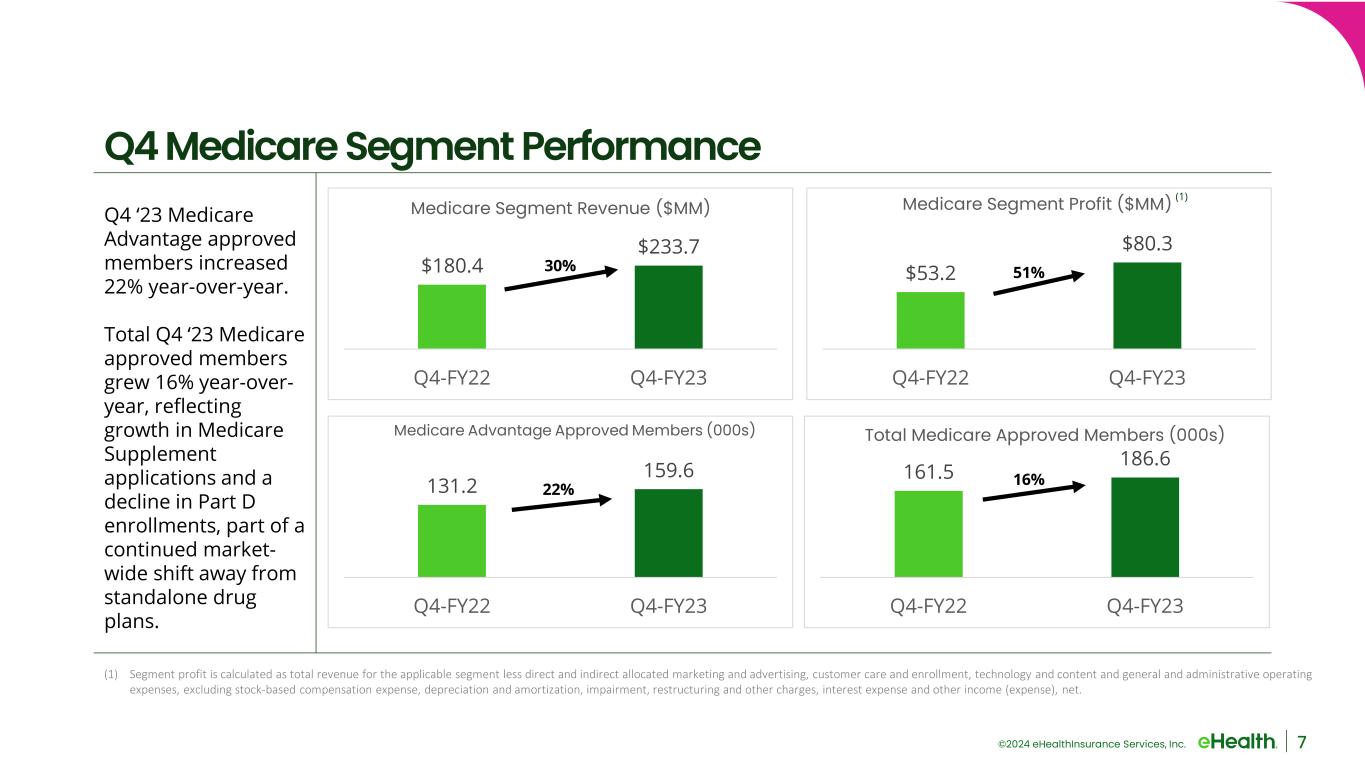
©2024 eHealthInsurance Services, Inc. Q4 ‘23 Medicare Advantage approved members increased 22% year-over-year. Total Q4 ‘23 Medicare approved members grew 16% year-over- year, reflecting growth in Medicare Supplement applications and a decline in Part D enrollments, part of a continued market- wide shift away from standalone drug plans. 7 Q4 Medicare Segment Performance (1) Segment profit is calculated as total revenue for the applicable segment less direct and indirect allocated marketing and advertising, customer care and enrollment, technology and content and general and administrative operating expenses, excluding stock-based compensation expense, depreciation and amortization, impairment, restructuring and other charges, and other income (expense), net. $180.4 $233.7 Q4-FY22 Q4-FY23 Medicare Segment Revenue ($MM) 30% $53.2 $80.3 Q4-FY22 Q4-FY23 Medicare Segment Profit ($MM) 51% 131.2 159.6 Q4-FY22 Q4-FY23 Medicare Advantage Approved Members (000s) 22% 161.5 186.6 Q4-FY22 Q4-FY23 Total Medicare Approved Members (000s) 16% (1) (1) Seg ent profit is calculated as total revenue for the applicable seg ent less direct and indirect allocated arketing and advertising, custo er care and enroll ent, technology and content and general and ad inistrative operating expenses, excluding stock-based co pensation expense, depreciation and a ortization, i pair ent, restructuring and other charges, interest expense and other income (expense), net.
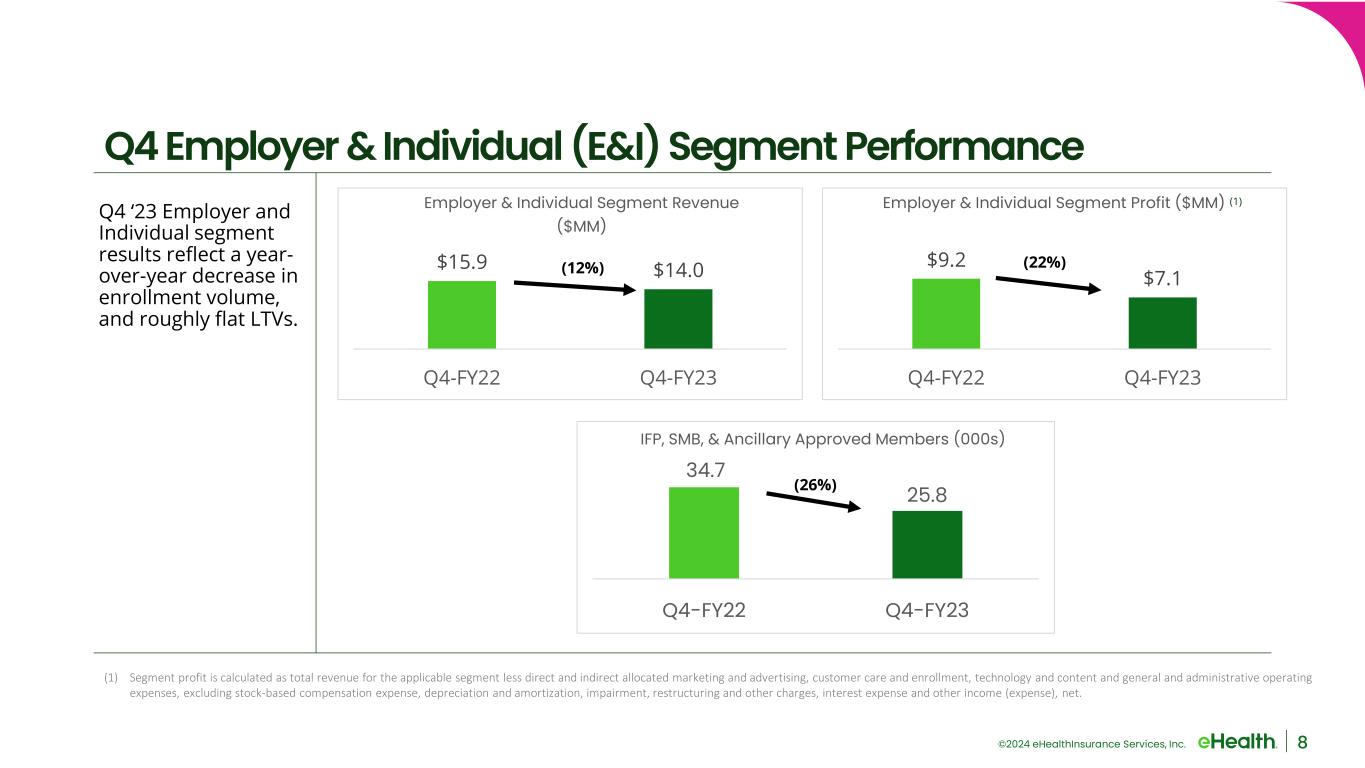
©2024 eHealthInsurance Services, Inc. Q4 ‘23 Employer and Individual segment results reflect a year- over-year decrease in enrollment volume, and roughly flat LTVs. 8 Q4 Employer & Individual (E&I) Segment Performance (1) Segment profit is calculated as total revenue for the applicable segment less direct and indirect allocated marketing and advertising, customer care and enrollment, technology and content and general and administrative operating expenses, excluding stock-based compensation expense, depreciation and amortization, impairment, restructuring and other charges, interest expense and other income (expense), net. (1) $15.9 $14.0 Q4-FY22 Q4-FY23 Employer & Individual Segment Revenue ($MM) (12%) 34.7 25.8 Q4-FY22 Q4-FY23 IFP, SMB, & Ancillary Approved Members (000s) (26%) $9.2 $7.1 Q4-FY22 Q4-FY23 Employer & Individual Segment Profit ($MM) (22%)

©2024 eHealthInsurance Services, Inc. 9 Local Markets Strategy Showing Strong Results Pilot in NY and IL markets Planned and prepared for full- scale deployment Rolled out local sales model agents across 6 markets Expanded program to 12 states Q1 2023 Q2 2023 Q4 2023 Q4 2022 • Born from the idea that “healthcare is local.” Aligned with local provider networks, pharmacies & strategic partners. • Seeing success in several metrics: Local market enrollments convert at higher rates and have a lower early cancelation rate than national enrollments. • In Q4 ‘23 Local Market agents converted 13% better relative to our national agents. • Plan to deepen our investment in existing local markets in 2024.

©2024 eHealthInsurance Services, Inc. Year-over-year growth in ending commissions receivable balance reflects Q4 enrollment growth and the upward revisions to our receivable that flowed through our income statement in the form of tail revenue. Fiscal 2023 operating cash flow improved year-over-year, driven by year-over-year improvements in operating cash flow Q1 through Q3 of 2023. 10 Cash Flow & Balance Sheet Highlights ($26.9) ($6.7) FY2022 FY2023 Operating Cash Flow ($MM) $144.4 $121.7 Dec 31, 2022 Dec 31, 2023 Ending Cash, Cash Equivalents & Marketable Securities ($MM) $884.3 $918.2 Dec 31, 2022 Dec 31, 2023 Ending Commissions Receivable (Current & Non-Current) ($MM)
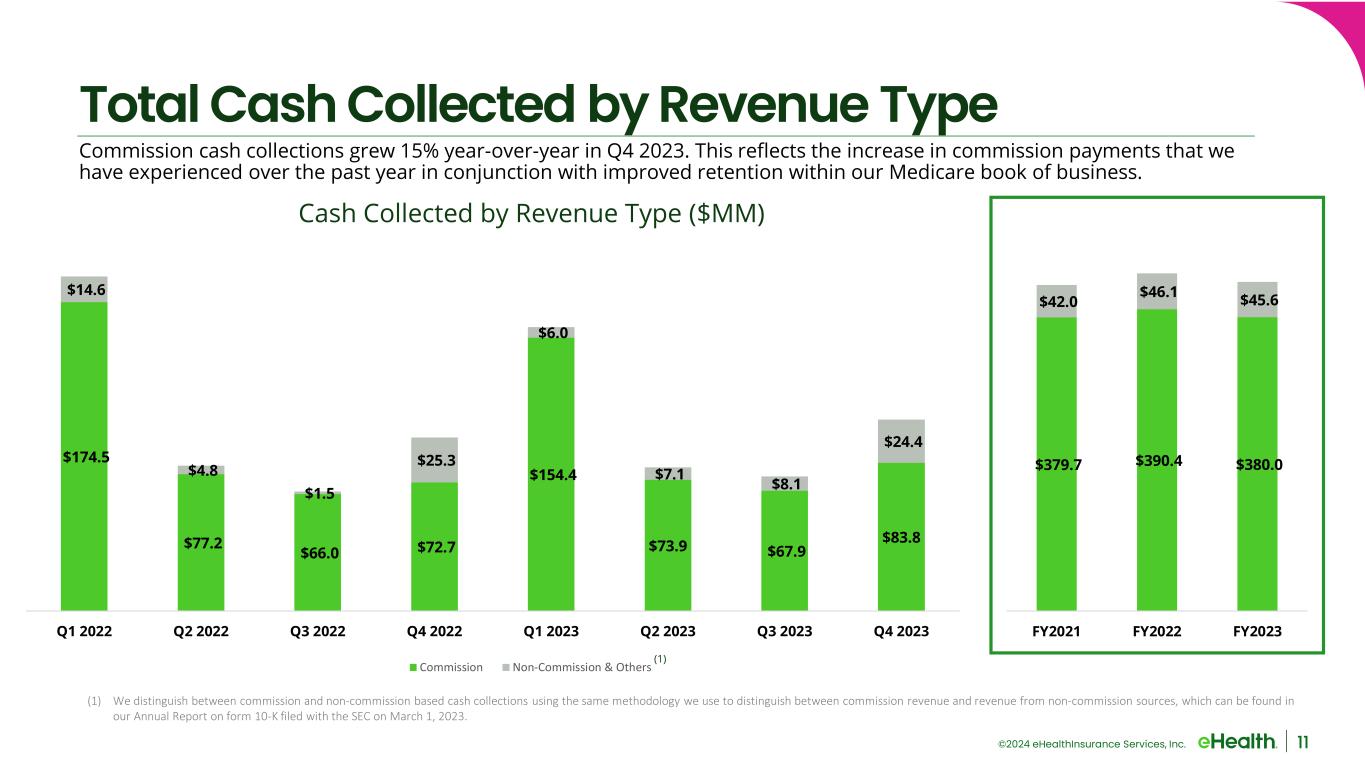
©2024 eHealthInsurance Services, Inc. $174.5 $77.2 $66.0 $72.7 $154.4 $73.9 $67.9 $83.8 $14.6 $4.8 $1.5 $25.3 $6.0 $7.1 $8.1 $24.4 Q1 2022 Q2 2022 Q3 2022 Q4 2022 Q1 2023 Q2 2023 Q3 2023 Q4 2023 Commission Non-Commission & Others $379.7 $390.4 $380.0 $42.0 $46.1 $45.6 FY2021 FY2022 FY2023 Total Cash Collected by Revenue Type Commission cash collections grew 15% year-over-year in Q4 2023. This reflects the increase in commission payments that we have experienced over the past year in conjunction with improved retention within our Medicare book of business. 11 (1) We distinguish between commission and non-commission based cash collections using the same methodology we use to distinguish between commission revenue and revenue from non-commission sources, which can be found in our Annual Report on form 10-K filed with the SEC on March 1, 2023. (1) Cash Collected by Revenue Type ($MM)

©2024 eHealthInsurance Services, Inc. 12 FY24 Operational Priorities Grow revenue year- over-year while producing positive adjusted EBITDA 1 Advance our local market focused, omni-channel enrollment engine to drive higher conversions and greater margins 2 Launch the next phase of our member loyalty & retention strategy 3 Drive our B2B strategy and fortify the organizational foundation that supports our strategic partners and direct-to- employer opportunities 4 Enhance eHealth’s comprehensive product portfolio beyond Medicare Advantage agency business to drive year- round growth 5
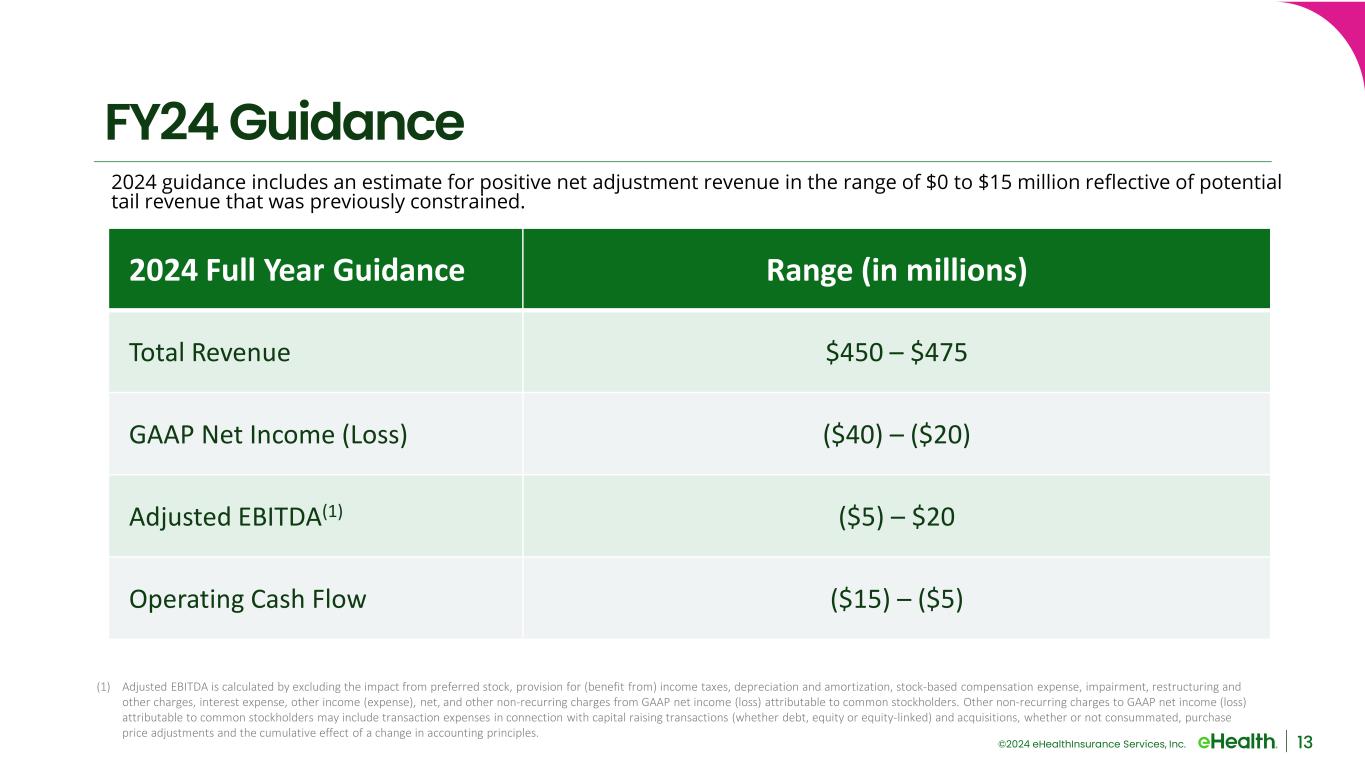
©2024 eHealthInsurance Services, Inc. 13 FY24 Guidance 2024 Full Year Guidance Range (in millions) Total Revenue $450 – $475 GAAP Net Income (Loss) ($40) – ($20) Adjusted EBITDA(1) ($5) – $20 Operating Cash Flow ($15) – ($5) (1) Adjusted EBITDA is calculated by excluding the impact from preferred stock, provision for (benefit from) income taxes, depreciation and amortization, stock-based compensation expense, impairment, restructuring and other charges, interest expense, other income (expense), net, and other non-recurring charges from GAAP net income (loss) attributable to common stockholders. Other non-recurring charges to GAAP net income (loss) attributable to common stockholders may include transaction expenses in connection with capital raising transactions (whether debt, equity or equity-linked) and acquisitions, whether or not consummated, purchase price adjustments and the cumulative effect of a change in accounting principles. 2024 guidance includes an estimate for positive net adjustment revenue in the range of $0 to $15 million reflective of potential tail revenue that was previously constrained.

©2024 eHealthInsurance Services, Inc. Appendix 14
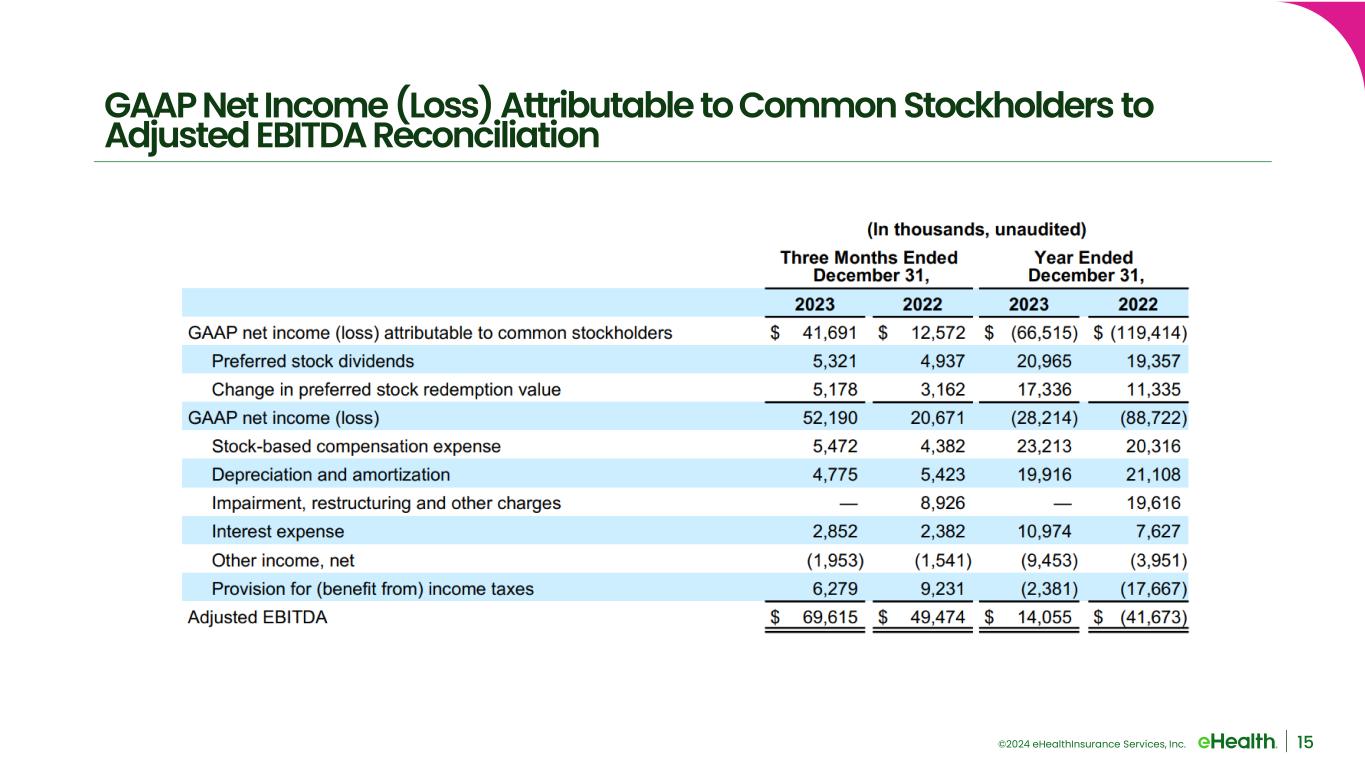
©2024 eHealthInsurance Services, Inc. 15 GAAP Net Income (Loss) Attributable to Common Stockholders to Adjusted EBITDA Reconciliation

©2024 eHealthInsurance Services, Inc. 16 Reconciliation of Non-GAAP Financial Measures to Guidance
v3.24.0.1
Cover Page
|
Feb. 27, 2024 |
| Cover [Abstract] |
|
| Document Type |
8-K
|
| Document Period End Date |
Feb. 27, 2024
|
| Entity Registrant Name |
EHEALTH, INC.
|
| Entity Incorporation, State or Country Code |
DE
|
| Entity File Number |
001-33071
|
| Entity Tax Identification Number |
56-2357876
|
| Entity Address, Address Line One |
13620 RANCH ROAD 620 N, SUITE A250
|
| Entity Address, City or Town |
AUSTIN
|
| Entity Address, State or Province |
TX
|
| Entity Address, Postal Zip Code |
78717
|
| City Area Code |
737
|
| Local Phone Number |
248-2340
|
| Written Communications |
false
|
| Soliciting Material |
false
|
| Pre-commencement Tender Offer |
false
|
| Title of 12(b) Security |
Common Stock, par value $0.001 per share
|
| Pre-commencement Issuer Tender Offer |
false
|
| Trading Symbol |
EHTH
|
| Security Exchange Name |
NASDAQ
|
| Entity Emerging Growth Company |
false
|
| Amendment Flag |
false
|
| Entity Central Index Key |
0001333493
|
| X |
- DefinitionBoolean flag that is true when the XBRL content amends previously-filed or accepted submission.
| Name: |
dei_AmendmentFlag |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionFor the EDGAR submission types of Form 8-K: the date of the report, the date of the earliest event reported; for the EDGAR submission types of Form N-1A: the filing date; for all other submission types: the end of the reporting or transition period. The format of the date is YYYY-MM-DD.
| Name: |
dei_DocumentPeriodEndDate |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:dateItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe type of document being provided (such as 10-K, 10-Q, 485BPOS, etc). The document type is limited to the same value as the supporting SEC submission type, or the word 'Other'.
| Name: |
dei_DocumentType |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:submissionTypeItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAddress Line 1 such as Attn, Building Name, Street Name
| Name: |
dei_EntityAddressAddressLine1 |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Definition
+ References
+ Details
| Name: |
dei_EntityAddressCityOrTown |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionCode for the postal or zip code
| Name: |
dei_EntityAddressPostalZipCode |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionName of the state or province.
| Name: |
dei_EntityAddressStateOrProvince |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:stateOrProvinceItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionA unique 10-digit SEC-issued value to identify entities that have filed disclosures with the SEC. It is commonly abbreviated as CIK. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityCentralIndexKey |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:centralIndexKeyItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionIndicate if registrant meets the emerging growth company criteria. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityEmergingGrowthCompany |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionCommission file number. The field allows up to 17 characters. The prefix may contain 1-3 digits, the sequence number may contain 1-8 digits, the optional suffix may contain 1-4 characters, and the fields are separated with a hyphen.
| Name: |
dei_EntityFileNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:fileNumberItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTwo-character EDGAR code representing the state or country of incorporation.
| Name: |
dei_EntityIncorporationStateCountryCode |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:edgarStateCountryItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe exact name of the entity filing the report as specified in its charter, which is required by forms filed with the SEC. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityRegistrantName |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe Tax Identification Number (TIN), also known as an Employer Identification Number (EIN), is a unique 9-digit value assigned by the IRS. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityTaxIdentificationNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:employerIdItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionLocal phone number for entity.
| Name: |
dei_LocalPhoneNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as pre-commencement communications pursuant to Rule 13e-4(c) under the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 13e
-Subsection 4c
| Name: |
dei_PreCommencementIssuerTenderOffer |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as pre-commencement communications pursuant to Rule 14d-2(b) under the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 14d
-Subsection 2b
| Name: |
dei_PreCommencementTenderOffer |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTitle of a 12(b) registered security. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b
| Name: |
dei_Security12bTitle |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:securityTitleItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionName of the Exchange on which a security is registered. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection d1-1
| Name: |
dei_SecurityExchangeName |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:edgarExchangeCodeItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as soliciting material pursuant to Rule 14a-12 under the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Section 14a
-Number 240
-Subsection 12
| Name: |
dei_SolicitingMaterial |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTrading symbol of an instrument as listed on an exchange.
| Name: |
dei_TradingSymbol |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:tradingSymbolItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as written communications pursuant to Rule 425 under the Securities Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Securities Act
-Number 230
-Section 425
| Name: |
dei_WrittenCommunications |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
eHealth (NASDAQ:EHTH)
Historical Stock Chart
From Mar 2024 to Apr 2024
eHealth (NASDAQ:EHTH)
Historical Stock Chart
From Apr 2023 to Apr 2024