By Peter Loftus
Diabetes patients are increasingly using electronic skin patches
and their phones, instead of pricking their fingers, to do the
complex job of managing a disease that affects more than 30 million
Americans.
The transformation in blood-sugar testing suggests how
harnessing technology and data may drive improvements for disease
management -- and profits for manufacturers.
Many patients now wear coin-sized skin patches on their arms or
abdomens that test for blood-sugar levels automatically, then send
the data to a patient's smartphone or even to a wearable insulin
pump that delivers the medicine.
Patients in the U.S. using the devices, known as
continuous-glucose monitors, numbered almost 840,000 as of March
31, more than double the 389,000 using them at the end of 2017,
according to Seagrove Partners LLC, a health-care research and
consulting firm.
Sales of the products are fueling growth at companies including
DexCom Inc., Abbott Laboratories and Medtronic PLC. Their sales of
the devices are expected to hit $3.2 billion this year, triple the
2016 total, according to JPMorgan Chase.
The market for the devices "is extremely large and growing
really fast," said Mike Hill, who heads the Medtronic unit selling
the sensors.
Tracking blood-sugar levels is vital for many diabetics, who
must regularly check if they are within healthy levels or need to
take insulin, sugar or some other medicine to avoid fainting or
worse. For years, many patients have had to prick their fingers
several times a day to draw blood and then insert the blood into a
meter for a reading.
Use of digital blood-sugar monitors, which first hit the market
in the mid-2000s, has soared in recent years partly because the
devices have become more accurate and more health plans are paying
for them.
"There's very few other diseases like this that put the bulk of
the data in the hands of the patient," said Aaron Kowalski, chief
executive of JDRF, a group that funds Type 1 diabetes research.
In Type 1 diabetes, the body doesn't produce insulin and
patients rely heavily on insulin therapy. In Type 2, the more
common type, the body doesn't use insulin properly.
With the connectivity linking monitors to smartphones and
insulin pumps come cybersecurity risks. The U.S. Food and Drug
Administration warned last month that certain models of Medtronic
insulin pumps could allow hackers to gain access, change settings
and cause patient harm.
Medtronic, which is recalling the pumps, said they were older
models and has recommended patients consider switching to newer
Medtronic models that have better cybersecurity protections.
The disposable sensors can be worn around the clock. They stick
to a patient's abdomen or arm and insert a tiny needle into the
skin to sense changes in blood sugar and transmit readings
wirelessly. Some patients have the glucose data sent to a wearable
insulin pump; some pumps can adjust the dose based on the glucose
reading.
Some monitors sound alarms and keep track of long-term data,
which patients can share with their physicians.
A DexCom-funded study published in JAMA in 2017 found that
patients using its monitor had greater decreases in average
blood-sugar levels than those using finger sticks and test
strips.
The data deluge, however, can overwhelm some patients,
especially new users. Some patients say they feel punished when the
monitor shows sugar levels are out of range and have asked for more
positive feedback when they stay in range, like a smiley face,
DexCom CEO Kevin Sayer said in an interview.
Raynham McArthur, a 14-year-old in Hamilton, Ontario, used to
wake up at midnight and 3 a.m. every night for her parents to take
blood samples. The multiple finger sticks left her fingers bruised
and sore.
Now, her sensor sends blood-sugar data to her parents' phones.
"I probably sleep through easily four nights a week," said her
mother, Joanna Wilson, a university science professor. She and her
husband, Andrew McArthur, monitor Raynham's sugar levels while she
is at school and text her to make sure she takes steps if the
numbers go out of range.
Raynham calls it "blood-sugar stalking." But the device made it
easier for her to go on a two-night school trip to Ottawa in June
without her parents. "It's a lot easier for me to go out and do
things with friends, " she said.
The cost, however, would be unaffordable for many patients who
lack insurance or whose insurer doesn't cover the devices, said
Mayer Davidson, a diabetes specialist at Charles R. Drew University
of Medicine and Science in Los Angeles.
Abbott's device, called FreeStyle Libre, costs around $1,308 a
year for the average patient; DexCom's system is about $3,000. With
insurance, the typical patient copay for Abbott's product is about
$31 a month, and $50 a month for DexCom's, said Erik Verhoef,
president of Seagrove Partners.
Competition for sales among device makers has been fierce.
Abbott priced its system at a significant discount to DexCom's to
grab an edge. Jared Watkin, senior vice president of Abbott's
diabetes-care unit, touts Libre's sensor, which lasts longer than
competitors'.
DexCom, which is working on a new version of its device with
Alphabet Inc.'s Verily unit, has been hiring data-analytics workers
to search for insights by pairing sugar data with exercise data
collected from other wearable devices, Mr. Sayer said.
Medtronic has used data collected from devices to develop
algorithms that predict when patients' blood-sugar levels will fall
too low, Mr. Hill said.
Write to Peter Loftus at peter.loftus@wsj.com
(END) Dow Jones Newswires
July 29, 2019 05:44 ET (09:44 GMT)
Copyright (c) 2019 Dow Jones & Company, Inc.
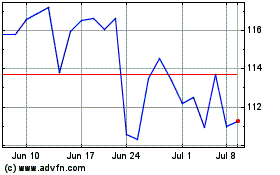
DexCom (NASDAQ:DXCM)
Historical Stock Chart
From Mar 2024 to Apr 2024
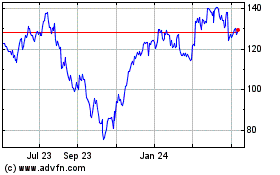
DexCom (NASDAQ:DXCM)
Historical Stock Chart
From Apr 2023 to Apr 2024