Molina Healthcare, Inc. (NYSE: MOH):
- Net income per diluted share for the
quarter of $0.58.
- Adjusted net income per diluted share
for the quarter of $0.67.
- Net income per diluted share for the
quarter up 35% over first quarter 2016.
- Adjusted net income per diluted share
for the quarter up 31% over first quarter 2016.
- Total revenue for the quarter of $4.4
billion, up 24% over second quarter 2015.
- Aggregate membership up 26% over second
quarter 2015.
Molina Healthcare, Inc. (NYSE: MOH) today reported its financial
results for the second quarter of 2016.
“The results we have reported today reflect meaningful progress
from the first quarter of 2016,” said J. Mario Molina, M.D., chief
executive officer of Molina Healthcare, Inc. “Last quarter, we
identified specific improvements that we needed to make to our
operations. Today’s announcement demonstrates that we are making
good headway with this work. The issues we identified in Ohio and
Texas in the first quarter are substantially resolved, and work in
Puerto Rico is well under way.”
Update on Financial
Performance
Second Quarter 2016 Compared With First Quarter 2016
Second quarter 2016 financial performance improved significantly
when compared with the first quarter of 2016. Earnings per diluted
share increased to $0.58 in the second quarter of 2016 from $0.43
in the first quarter. Adjusted earnings per diluted share increased
to $0.67 in the second quarter of 2016 from $0.51 in the first
quarter.
Higher profitability in the second quarter was primarily the
result of improvements at the Ohio and Texas health plans. The
medical care ratio of the Ohio health plan decreased to 89.7% in
the second quarter of 2016 from 92.0% in the first quarter. The
medical care ratio of the Texas health plan decreased to 78.5% in
the second quarter of 2016 from 92.8% in the first quarter. Even
without the benefit of out-of-period quality revenue adjustments
discussed below, the medical care ratio of the Texas health plan
would have been approximately 85.3% in the second quarter, still
well under the 92.8% medical care ratio reported in the first
quarter.
In total, out-of-period adjustments related to 2015 dates of
service were not significant to second quarter performance.
Out-of-period adjustments were significant, however, on a
geographic and program basis. Out-of-period adjustments were the
result of changes in accounting estimates made as new information
became available to the Company. The table below will help the
reader to understand the discussion that follows.
Summary of
Significant Out-of-Period Adjustments Affecting 2016 Financial
Results
Three Months Ended Six Months
Ended June 30, 2016 June 30, 2016 (In
millions, except per diluted share amounts) Amount
Per Diluted
Share
Amount
Per Diluted
Share
Marketplace adjustments for 2015 dates of service $ (37 ) $ (0.42 )
$ (68 ) $ (0.76 )
Texas quality revenue adjustment for
2014/2015 dates of service
44 0.50 44 0.49 Texas quality revenue adjustment for 1Q 2016 dates
of service 7 0.08 N/A N/A Puerto Rico premium revenue adjustment
for 2015 dates of service (11 ) (0.12 ) (11 ) (0.12 ) Florida
premium revenue adjustment for 2014/2015 dates of service —
— 18 0.20 Total out-of-period adjustments, net
$ 3 $ 0.04 $ (17 ) $ (0.19 )
Out-of-period adjustments increased pretax income by
approximately $3 million (or approximately $0.04 per diluted share)
in the second quarter of 2016. Specifically:
- Adjustments related to 2015 dates of
service reduced Marketplace pretax income by approximately $37
million (or approximately $0.42 per diluted share) in the second
quarter. On June 30, 2016, the Centers for Medicare and Medicaid
Services released the final update on risk adjustment and
reinsurance payments for the 2015 benefit year, and we adjusted our
accruals accordingly.
- During the second quarter, we were
informed by the Texas Department of Health and Human Services that
it will not recoup any quality revenue for calendar years 2014,
2015, and 2016. Therefore, we recognized previously deferred
quality revenue amounting to approximately $51 million (or
approximately $0.58 per diluted share) in the second quarter of
2016. Of the $51 million adjustment, $44 million related to 2015
and 2014 dates of service, and $7 million related to the first
quarter of 2016.
- Reductions to revenue previously
recorded for 2015 dates of service in Puerto Rico decreased pretax
income by approximately $11 million (or approximately $0.12 per
diluted share) in the second quarter.
Understanding the First Half of 2016
We reported pretax income of $144 million for the first half of
2016. These results were affected by several out-of-period
adjustments related to dates of service in 2015 and 2014. In total,
these adjustments reduced pretax income in the first half of 2016
by approximately $17 million (or approximately $0.19 per diluted
share). Specifically:
- Adjustments related to 2015 dates of
service reduced Marketplace pretax income by approximately $68
million (or approximately $0.76 per diluted share) in the first
half of 2016. We now estimate that the medical care ratio for our
Marketplace program for all of 2015 was approximately 80%. Through
June 30, 2016, the medical care ratio of our Marketplace program
for months of service in the first half of 2016 alone (exclusive of
out-of-period adjustments) was approximately 78%.
- As described above, the recognition of
Texas quality revenue associated with calendar years 2014 and 2015
increased pretax income in the first half of 2016 by approximately
$44 million (or approximately $0.49 per diluted share).
- Also as noted above, reductions to 2015
premium revenue in Puerto Rico reduced pretax income by
approximately $11 million (or approximately $0.12 per diluted
share) in the first half of 2016.
- Retroactive adjustments to premium
revenue in Florida for dates of service in 2014 and 2015 increased
pretax income by approximately $18 million (or approximately $0.20
per diluted share) in the first half of 2016. Prior to reporting
first quarter 2016 results, we were informed by the Florida Agency
for Health Care Administration that we were due a retroactive
increase to Medicaid premium revenue relating to dates of service
prior to 2016. We reported this development in our first quarter
2016 results.
Net Income per Share Guidance
Our net income per share guidance for fiscal year 2016 remains
unchanged. We expect the following factors, among others, to affect
our financial performance in the second half of 2016:
- The ultimate savings to be realized
from various cost savings initiatives and the speed at which such
savings will be realized.
- Medicaid rate increases (excluding
Medicaid Expansion) of approximately 3.0% in California (effective
July 1, 2016); approximately 2.5% in Puerto Rico (effective July 1,
2016); and approximately 3.0% in Texas (effective September 1,
2016). All rate changes are consistent with our previous
expectations.
- Medicaid Expansion rate decreases of
approximately 11.0% in California (effective July 1, 2016) and
approximately 2.0% in Ohio (effective July 1, 2016). All rate
changes are consistent with our previous expectations.
- The implementation of a medical care
ratio floor of 86.0% for the South Carolina Medicaid program
effective July 1, 2016.
- Declining margins for our Marketplace
business during the second half of 2016 due to normal membership
attrition; the addition of higher cost members through the special
enrollment process; higher costs as members reach the limits of the
cost-sharing provisions of their insurance coverage; and increasing
utilization as members become more engaged with our care networks.
This is consistent with our previous expectations.
Conference Call
Management will host a conference call and webcast to discuss
Molina Healthcare's second quarter results at 5:00 p.m. Eastern
time on Wednesday, July 27, 2016. The number to call for the
interactive teleconference is (212) 271-4651. A telephonic replay
of the conference call will be available from 7:00 p.m. Eastern
time on Wednesday, July 27, 2016, through 6:00 p.m. Eastern Time on
Thursday, July 28, 2016, by dialing (800) 633-8284 and entering
confirmation number 21812476. A live audio broadcast of Molina
Healthcare’s conference call will be available on our website,
molinahealthcare.com. A 30-day online
replay will be available approximately an hour following the
conclusion of the live broadcast.
About Molina Healthcare
Molina Healthcare, Inc., a FORTUNE 500 company, provides managed
health care services under the Medicaid and Medicare programs and
through the state insurance marketplaces. Through our locally
operated health plans in 11 states across the nation and in the
Commonwealth of Puerto Rico, Molina currently serves approximately
4.2 million members. Dr. C. David Molina founded our company in
1980 as a provider organization serving low-income families in
Southern California. Today, we continue his mission of providing
high quality and cost-effective health care to those who need it
most. For more information about Molina Healthcare, please visit
our website at molinahealthcare.com.
Safe Harbor Statement under the Private Securities Litigation
Reform Act of 1995: This earnings release contains
“forward-looking statements” regarding our plans, expectations, and
anticipated future events. Actual results could differ materially
due to numerous known and unknown risks and uncertainties. Those
known risks and uncertainties include, but are not limited to, the
following:
- the success of our profit improvement
and cost-cutting initiatives;
- uncertainties and evolving market and
provider economics associated with the implementation of the
Affordable Care Act (the “ACA”), the Medicaid expansion, the
insurance marketplaces, the effect of various implementing
regulations, and uncertainties regarding the Medicare-Medicaid dual
eligible demonstration programs in California, Illinois, Michigan,
Ohio, South Carolina, and Texas;
- management of our medical costs,
including our ability to reduce over time the high medical costs
commonly associated with new patient populations;
- our ability to predict with a
reasonable degree of accuracy utilization rates, including
utilization rates in new plans, geographies, and programs where we
have less experience with patient and provider populations, and
also including utilization rates associated with seasonal flu
patterns or other newly emergent diseases;
- our ability to manage growth, including
maintaining and creating adequate internal systems and controls
relating to authorizations, approvals, provider payments, and the
overall success of our care management initiatives designed to
control costs;
- our receipt of adequate premium rates
to support increasing pharmacy costs, including costs associated
with specialty drugs and costs resulting from formulary changes
that allow the option of higher-priced non-generic drugs;
- our ability to operate profitably in an
environment where the trend in premium rate increases lags behind
the trend in increasing medical costs;
- the interpretation and implementation
of federal or state medical cost expenditure floors, administrative
cost and profit ceilings, premium stabilization programs, profit
sharing arrangements, and risk adjustment provisions;
- the interpretation and implementation
of at-risk premium rules regarding the achievement of certain
quality measures, and our ability to recognize revenue amounts
associated therewith;
- the interpretation and implementation
of state contract performance requirements regarding the
achievement of certain quality measures, and our ability to avoid
liquidated damages associated therewith;
- cyber-attacks or other privacy or data
security incidents resulting in an inadvertent unauthorized
disclosure of protected health information;
- the success of our health plan in
Puerto Rico, including the resolution of the Puerto Rico debt
crisis, payment of all amounts due under our Medicaid contract, the
effect of the newly enacted PROMESA law, and our efforts to better
manage the health care costs of our Puerto Rico health plan;
- significant budget pressures on state
governments and their potential inability to maintain current
rates, to implement expected rate increases, or to maintain
existing benefit packages or membership eligibility thresholds or
criteria, including the resolution of the Illinois budget impasse
and continued payment of all amounts due to our Illinois health
plan;
- the accurate estimation of incurred but
not reported or paid medical costs across our health plans;
- subsequent adjustments to reported
premium revenue based upon subsequent developments or new
information, including changes to estimated amounts due to or
receivable from CMS under the ACA's “three R’s” marketplace premium
stabilization programs;
- efforts by states to recoup previously
paid amounts, including our dispute with the state of New Mexico
related to reimbursement for retroactively enrolled members in
2014;
- the success of our efforts to retain
existing government contracts and to obtain new government
contracts in connection with state requests for proposals (RFPs) in
both existing and new states;
- the continuation and renewal of the
government contracts of our health plans, Molina Medicaid
Solutions, and Pathways, and the terms under which such contracts
are renewed;
- complications, member confusion, or
enrollment backlogs related to the annual renewal of Medicaid
coverage;
- government audits and reviews, and any
fine, enrollment freeze, or monitoring program that may result
therefrom;
- changes with respect to our provider
contracts and the loss of providers;
- approval by state regulators of
dividends and distributions by our health plan subsidiaries;
- changes in funding under our contracts
as a result of regulatory changes, programmatic adjustments, or
other reforms;
- high dollar claims related to
catastrophic illness;
- the favorable resolution of litigation,
arbitration, or administrative proceedings;
- the relatively small number of states
in which we operate health plans;
- the effect on our Los Angeles County
subcontract of Centene Corporation’s acquisition of Health Net
Inc.;
- the availability of adequate financing
on acceptable terms to fund and capitalize our expansion and
growth, repay our outstanding indebtedness at maturity and meet our
liquidity needs, including the interest expense and other costs
associated with such financing;
- the failure of a state in which we
operate to renew its federal Medicaid waiver;
- changes generally affecting the managed
care or Medicaid management information systems industries;
- increases in government surcharges,
taxes, and assessments, including but not limited to the
deductibility of certain compensation costs;
- newly emergent viruses or widespread
epidemics, including the Zika virus, public catastrophes or
terrorist attacks, and associated public alarm;
- changes in general economic conditions,
including unemployment rates;
- the sufficiency of our funds on hand to
pay the amounts due upon conversion of our outstanding notes;
- increasing competition and
consolidation in the Medicaid industry;
and numerous other risk factors, including those discussed in
our periodic reports and filings with the Securities and Exchange
Commission. These reports can be accessed under the investor
relations tab of our website or on the SEC’s website at
sec.gov. Given these risks and
uncertainties, we can give no assurances that our forward-looking
statements will prove to be accurate, or that any other results or
events projected or contemplated by our forward-looking statements
will in fact occur, and we caution investors not to place undue
reliance on these statements. All forward-looking statements in
this release represent our judgment as of July 27, 2016, and we
disclaim any obligation to update any forward-looking statements to
conform the statement to actual results or changes in our
expectations.
MOLINA HEALTHCARE, INC.
UNAUDITED CONSOLIDATED STATEMENTS OF
INCOME
Three Months Ended June 30, Six Months Ended June
30, 2016 2015 2016
2015 (Dollar amounts in millions, except net
income per share) Revenue: Premium revenue $ 4,029 $ 3,304 $
8,024 $ 6,275 Service revenue 135 47 275 99 Premium tax revenue 109
95 218 190 Health insurer fee revenue 76 74 166 122 Investment
income 8 4 16 7 Other revenue 2 1 3 3
Total revenue 4,359 3,525 8,702 6,696
Operating expenses: Medical care costs 3,594 2,929 7,182 5,565 Cost
of service revenue 116 33 243 69 General and administrative
expenses 351 287 691 543 Premium tax expenses 109 95 218 190 Health
insurer fee expenses 50 40 108 81 Depreciation and amortization 34
25 66 50 Total operating expenses 4,254
3,409 8,508 6,498 Operating income 105
116 194 198 Interest expense 25 15 50 30
Income before income tax expense 80 101 144 168 Income tax
expense 47 62 87 101 Net income $ 33
$ 39 $ 57 $ 67 Diluted net
income per share $ 0.58 $ 0.72 $ 1.01 $ 1.29
Diluted weighted average shares outstanding 55.5
53.9 56.3 52.0
Operating
Statistics: Medical care ratio (1) 89.2 % 88.7 % 89.5 % 88.7 %
General and administrative expense ratio (2) 8.1 % 8.1 % 7.9 % 8.1
% Premium tax ratio (1) 2.6 % 2.8 % 2.6 % 2.9 % Effective tax rate
59.8 % 61.3 % 60.7 % 60.1 % Net profit margin (2) 0.7 % 1.1 % 0.7 %
1.0 % (1) Medical care ratio represents medical care costs
as a percentage of premium revenue; premium tax ratio represents
premium tax expenses as a percentage of premium revenue plus
premium tax revenue. (2) Computed as a percentage of total revenue.
MOLINA HEALTHCARE, INC.
UNAUDITED CONSOLIDATED BALANCE
SHEETS
June 30, December 31, 2016 2015
(Unaudited) (Amounts in millions,except per-share
data) ASSETS Current assets: Cash and cash equivalents $
2,345 $ 2,329 Investments 1,968 1,801 Receivables 1,012 597 Income
taxes refundable 23 13 Prepaid expenses and other current assets
197 192 Derivative asset — 374 Total current assets
5,545 5,306 Property, equipment, and capitalized software, net 448
393 Deferred contract costs 80 81 Intangible assets, net 146 122
Goodwill 611 519 Restricted investments 107 109 Deferred income
taxes — 18 Derivative asset 226 — Other assets 39 28
$ 7,202 $ 6,576
LIABILITIES AND
STOCKHOLDERS’ EQUITY Current liabilities: Medical claims and
benefits payable $ 1,766 $ 1,685 Amounts due government agencies
1,238 729 Accounts payable and accrued liabilities 537 362 Deferred
revenue 104 223 Current portion of long-term debt 1 449 Derivative
liability — 374 Total current liabilities 3,646 3,822
Senior notes 1,428 962 Lease financing obligations 198 198 Deferred
income taxes 25 — Derivative liability 226 — Other long-term
liabilities 38 37 Total liabilities 5,561
5,019 Stockholders’ equity: Common stock, $0.001 par value;
150 shares authorized; outstanding: 57 shares at June 30, 2016 and
56 shares at December 31, 2015 — — Preferred stock, $0.001 par
value; 20 shares authorized, no shares issued and outstanding — —
Additional paid-in capital 822 803 Accumulated other comprehensive
gain (loss) 4 (4 ) Retained earnings 815 758 Total
stockholders’ equity 1,641 1,557 $ 7,202 $
6,576
MOLINA HEALTHCARE, INC.
UNAUDITED CONDENSED CONSOLIDATED
STATEMENTS OF CASH FLOWS
Three Months Ended June 30, Six Months Ended June
30, 2016 2015 2016
2015 (Amounts in millions) Operating
activities: Net income $ 33 $ 39 $ 57 $ 67 Adjustments to reconcile
net income to net cash provided by operating activities:
Depreciation and amortization 45 29 89 62 Deferred income taxes 9 6
39 7 Share-based compensation 9 3 16 9 Amortization of convertible
senior notes and lease financing obligations 7 8 15 15 Other, net 5
6 11 9 Changes in operating assets and liabilities: Receivables
(149 ) (140 ) (415 ) (35 ) Prepaid expenses and other assets 59 40
(143 ) (97 ) Medical claims and benefits payable (173 ) 44 82 292
Amounts due government agencies 328 203 509 298 Accounts payable
and accrued liabilities (58 ) (31 ) 147 158 Deferred revenue 10
(112 ) (119 ) (138 ) Income taxes 14 (1 ) (10 ) 1 Net
cash provided by operating activities 139 94 278
648 Investing activities: Purchases of
investments (363 ) (555 ) (974 ) (993 ) Proceeds from sales and
maturities of investments 464 286 812 541 Purchases of property,
equipment, and capitalized software (56 ) (41 ) (102 ) (66 )
Change in restricted investments
9 (9 ) 5 (14 ) Net cash paid in business combinations (6 ) — (8 )
(8 ) Other, net (7 ) (10 ) (6 ) (17 ) Net cash provided by (used
in) investing activities 41 (329 ) (273 ) (557 )
Financing activities: Proceeds from common stock offering, net of
issuance costs — 373 — 373 Proceeds from employee stock plans 10 7
10 8 Other, net (1 ) (1 ) 1 3 Net cash provided by
financing activities 9 379 11 384 Net
increase in cash and cash equivalents 189 144 16 475 Cash and cash
equivalents at beginning of period 2,156 1,870 2,329
1,539 Cash and cash equivalents at end of period $
2,345 $ 2,014 $ 2,345 $ 2,014
MOLINA HEALTHCARE, INC.UNAUDITED
NON-GAAP FINANCIAL MEASURES
We use two non-GAAP financial measures as supplemental metrics
in evaluating our financial performance, making financing and
business decisions, and forecasting and planning for future
periods. For these reasons, management believes such measures are
useful supplemental measures to investors in comparing our
performance to the performance of other public companies in the
health care industry. These non-GAAP financial measures should be
considered as supplements to, and not as substitutes for or
superior to, GAAP measures.
The first of these non-GAAP measures is earnings before
interest, taxes, depreciation and amortization (EBITDA). We believe
that EBITDA is particularly helpful in assessing our ability to
meet the cash demands of our operating units. The following table
reconciles net income, which we believe to be the most comparable
GAAP measure, to EBITDA.
Three Months Ended June 30,
Six Months Ended June 30, 2016
2015 2016 2015 (Amounts in
millions) Net income $ 33 $ 39 $ 57 $ 67 Adjustments:
Depreciation, and amortization of intangible assets and capitalized
software 39 29 76 58 Interest expense 25 15 50 30 Income tax
expense 47 62 87 101 EBITDA $ 144 $ 145
$ 270 $ 256
The second of these non-GAAP measures is adjusted net income
(including adjusted net income per diluted share). We believe that
adjusted net income per diluted share is very helpful in assessing
our financial performance exclusive of the non-cash impact of the
amortization of purchased intangibles. The following table
reconciles net income, which we believe to be the most comparable
GAAP measure, to adjusted net income.
Three Months Ended June 30,
Six Months Ended June 30, 2016
2015 2016 2015 (In millions,
except per diluted share amounts) Amount
Per share Amount Per share
Amount Per share Amount
Per share Net income $ 33 $ 0.58 $ 39 $ 0.72 $ 57 $
1.01 $ 67 $ 1.29 Adjustment, net of tax: Amortization of intangible
assets 5 0.09 3 0.05 10 0.17
6 0.10 Adjusted net income $ 38 $ 0.67
$ 42 $ 0.77 $ 67 $ 1.18 $ 73 $
1.39
MOLINA HEALTHCARE, INC.
UNAUDITED HEALTH PLANS SEGMENT
MEMBERSHIP
June 30, March 31, December 31, June
30, 2016 2016 2015 2015 Ending
Membership by Health Plan: California 680,000 676,000 620,000
593,000 Florida 565,000 576,000 440,000 348,000 Illinois 201,000
206,000 98,000 101,000 Michigan 393,000 399,000 328,000 260,000 New
Mexico 251,000 246,000 231,000 225,000 Ohio 341,000 336,000 327,000
332,000
Puerto Rico
336,000 339,000 348,000 361,000 South Carolina 105,000 102,000
99,000 114,000 Texas 367,000 380,000 260,000 266,000 Utah 151,000
151,000 102,000 92,000 Washington 709,000 672,000 582,000 553,000
Wisconsin 134,000 137,000 98,000 107,000
4,233,000 4,220,000 3,533,000 3,352,000
Ending Membership by Program:
Temporary Assistance for Needy Families
(TANF), CHIP(1)
2,500,000 2,485,000 2,312,000 2,180,000 Medicaid Expansion 654,000
632,000 557,000 475,000 Marketplace 597,000 630,000 205,000 261,000
Aged, Blind or Disabled (ABD) 387,000 380,000 366,000 353,000
Medicare-Medicaid Plan (MMP) - Integrated 51,000 50,000 51,000
39,000 Medicare Special Needs Plans 44,000 43,000
42,000 44,000 4,233,000 4,220,000 3,533,000
3,352,000
(1) CHIP stands for Children’s Health
Insurance Program.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA
(In millions, except percentages and
per-member per-month amounts)
Three Months Ended June 30, 2016
Member
Months(1)
Premium Revenue Medical Care
Costs MCR(2)
Medical Margin Total PMPM
Total PMPM California 2.0 $ 554 $
268.95 $ 493 $ 239.63 89.1 % $ 61 Florida 1.8 464 273.90 426 251.69
91.9 38 Illinois 0.6 154 256.17 137 227.71 88.9 17 Michigan 1.2 369
312.18 334 282.86 90.6 35 New Mexico 0.8 342 451.72 305 403.52 89.3
37 Ohio 1.0 483 473.91 433 424.87 89.7 50 Puerto Rico 1.0 170
169.04 175 173.49 102.6 (5 ) South Carolina 0.3 87 277.22 71 226.27
81.6 16 Texas 1.1 635 571.14 499 448.23 78.5 136 Utah 0.5 110
240.26 106 233.12 97.0 4 Washington 2.1 559 264.40 500 236.32 89.4
59 Wisconsin 0.4 99 244.88 96 235.88 96.3 3 Other(3) — 3
— 19 — — (16 ) 12.8 $ 4,029 $ 316.72 $
3,594 $ 282.54 89.2 % $ 435
Three Months
Ended June 30, 2015 Member
Months(1)
Premium Revenue Medical Care Costs
MCR(2) Medical Margin Total PMPM
Total PMPM California 1.7 $ 503 $ 285.14 $ 459 $
259.85 91.1 % $ 44 Florida 1.1 257 244.35 217 205.97 84.3 40
Illinois 0.3 102 337.55 98 325.91 96.6 4 Michigan 0.8 237 307.27
200 258.67 84.2 37 New Mexico 0.7 322 466.46 276 400.27 85.8 46
Ohio 1.1 509 510.30 432 433.75 85.0 77 Puerto Rico 1.1 194 179.33
184 170.32 95.0 10 South Carolina 0.4 93 276.36 67 196.92 71.3 26
Texas 0.8 512 635.74 468 581.42 91.5 44 Utah 0.2 80 288.60 72
258.88 89.7 8 Washington 1.6 410 249.39 371 225.46 90.4 39
Wisconsin 0.3 75 233.15 56 175.62 75.3 19 Other(3) — 10
— 29 — — (19 ) 10.1 $ 3,304 $ 328.96 $
2,929 $ 291.65 88.7 % $ 375 (1) A
member month is defined as the aggregate of each month’s ending
membership for the period presented. (2) The MCR represents medical
costs as a percentage of premium revenue. (3) “Other” medical care
costs include primarily medically related administrative costs at
the parent company, and direct delivery costs.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA
(In millions, except percentages and
per-member per-month amounts)
Six Months Ended June 30, 2016 Member
Months(1)
Premium Revenue Medical Care
Costs MCR(2)
Medical Margin Total PMPM
Total PMPM California 4.0 $ 1,095 $
271.14 $ 962 $ 238.30 87.9 % $ 133 Florida 3.4 953 284.53 839
250.58 88.1 114 Illinois 1.2 303 261.43 269 232.06 88.8 34 Michigan
2.4 756 316.18 681 285.13 90.2 75 New Mexico 1.5 678 450.62 601
399.17 88.6 77 Ohio 2.0 971 481.44 882 437.35 90.8 89 Puerto Rico
2.0 351 172.98 349 171.95 99.4 2 South Carolina 0.6 171 276.61 138
223.58 80.8 33 Texas 2.2 1,255 575.87 1,074 492.65 85.5 181 Utah
0.9 224 252.08 208 234.46 93.0 16 Washington 4.1 1,065 260.05 958
233.84 89.9 107 Wisconsin 0.8 196 247.57 188 236.92 95.7 8 Other(3)
— 6 — 33 — — (27 ) 25.1 $ 8,024
$ 320.17 $ 7,182 $ 286.57 89.5 % $ 842
Six
Months Ended June 30, 2015 Member
Months(1)
Premium Revenue Medical Care Costs
MCR(2) Medical Margin Total PMPM
Total PMPM California 3.4 $ 1,014 $ 294.85 $ 911 $
264.97 89.9 % $ 103 Florida 2.0 568 291.33 498 255.45 87.7 70
Illinois 0.6 206 339.72 188 309.66 91.2 18 Michigan 1.5 457 298.87
385 251.57 84.2 72 New Mexico 1.4 636 462.62 568 413.48 89.4 68
Ohio 2.1 1,024 498.96 845 412.05 82.6 179 Puerto Rico 1.1 194
179.33 184 170.32 95.0 10 South Carolina 0.7 184 271.35 141 206.88
76.2 43 Texas 1.6 894 565.45 820 518.60 91.7 74 Utah 0.5 157 289.42
146 268.72 92.8 11 Washington 3.2 786 245.22 723 225.47 91.9 63
Wisconsin 0.6 135 216.85 105 168.58 77.7 30 Other(3) — 20
— 51 — — (31 ) 18.7 $ 6,275 $ 336.21 $
5,565 $ 298.18 88.7 % $ 710 (1) A
member month is defined as the aggregate of each month’s ending
membership for the period presented. (2) The MCR represents medical
costs as a percentage of premium revenue. (3) “Other” medical care
costs include primarily medically related administrative costs at
the parent company, and direct delivery costs.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA
(In millions, except percentages and
per-member per-month amounts)
Three Months Ended June 30, 2016 Member
Months(1)
Premium Revenue Medical Care
Costs MCR(2)
Medical
Margin
Total PMPM Total
PMPM TANF and CHIP 7.5 $ 1,302 $ 173.57 $ 1,202 $ 160.26
92.3 % $ 100 Medicaid Expansion 1.9 742 378.19 634 323.56 85.6 108
Marketplace 1.8 373 206.88 323 178.79 86.4 50 ABD 1.2 1,168 991.38
1,038 881.80 88.9 130 MMP 0.2 315 2,093.29 270 1,792.78 85.6 45
Medicare 0.2 129 997.44 127 974.30 97.7 2
12.8 $ 4,029 $ 316.72 $ 3,594 $ 282.54
89.2 % $ 435
Three Months Ended June 30, 2015
Member
Months(1)
Premium Revenue Medical Care Costs
MCR(2)
Medical
Margin
Total PMPM Total PMPM TANF and CHIP 6.5
$ 1,169 $ 178.38 $ 1,063 $ 162.24 91.0 % $ 106 Medicaid Expansion
1.4 582 419.67 474 341.67 81.4 108 Marketplace 0.8 161 204.22 90
113.21 55.4 71 ABD 1.1 1,053 984.99 947 885.84 89.9 106 MMP 0.1 198
1,784.30 214 1,934.40 108.4 (16 ) Medicare 0.2 141
1,059.90 141 1,062.71 100.3 — 10.1 $
3,304 $ 328.96 $ 2,929 $ 291.65 88.7 % $ 375
Six Months Ended June 30, 2016 Member
Months(1)
Premium Revenue Medical Care Costs
MCR(2)
Medical
Margin
Total PMPM Total PMPM TANF and CHIP
14.9 $ 2,626 $ 176.00 $ 2,400 $ 160.85 91.4 % $ 226 Medicaid
Expansion 3.8 1,421 371.82 1,208 316.13 85.0 213 Marketplace 3.4
782 228.19 657 191.62 84.0 125 ABD 2.4 2,280 976.58 2,079 890.71
91.2 201 MMP 0.3 655 2,157.55 587 1,932.73 89.6 68 Medicare 0.3
260 1,013.04 251 977.35 96.5 9 25.1
$ 8,024 $ 320.17 $ 7,182 $ 286.57 89.5 % $ 842
Six Months Ended June 30, 2015 Member
Months(1)
Premium Revenue Medical Care Costs
MCR(2)
Medical
Margin
Total PMPM Total PMPM TANF and CHIP
12.0 $ 2,141 $ 177.93 $ 1,960 $ 162.89 91.6 % $ 181 Medicaid
Expansion 2.7 1,089 409.29 867 325.84 79.6 222 Marketplace 1.4 355
258.66 246 179.15 69.3 109 ABD 2.1 1,993 940.23 1,810 853.56 90.8
183 MMP 0.2 423 1,986.04 413 1,942.20 97.8 10 Medicare 0.3
274 1,036.95 269 1,020.01 98.4 5 18.7 $
6,275 $ 336.21 $ 5,565 $ 298.18 88.7 % $ 710
(1) A member month is defined as the aggregate of
each month’s ending membership for the period presented. (2) The
MCR represents medical costs as a percentage of premium revenue.
MOLINA HEALTHCARE, INC. UNAUDITED
SELECTED HEALTH PLANS SEGMENT FINANCIAL DATA (In millions,
except percentages and per-member per-month amounts)
The following tables provide the details
of our medical care costs for the periods indicated:
Three Months Ended June 30, 2016
2015 Amount PMPM
% of
Total
Amount PMPM % of
Total
Fee for service $ 2,620 $ 206.01 72.9 % $ 2,103 $ 209.34 71.8 %
Pharmacy 529 41.59 14.7 392 39.01 13.3 Capitation 304 23.87 8.5 248
24.72 8.5 Direct delivery 18 1.39 0.5 27 2.78 1.0 Other 123
9.68 3.4 159 15.80 5.4 $ 3,594
$ 282.54 100.0 % $ 2,929 $ 291.65 100.0
%
Six Months Ended June 30, 2016 2015
Amount PMPM % of
Total
Amount PMPM % of
Total
Fee for service $ 5,357 $ 213.77 74.6 % $ 4,051 $ 217.05 72.8 %
Pharmacy 1,054 42.05 14.7 743 39.81 13.4 Capitation 599 23.87 8.3
465 24.90 8.3 Direct delivery 34 1.36 0.5 54 2.93 1.0 Other 138
5.52 1.9 252 13.49 4.5 $
7,182 $ 286.57 100.0 % $ 5,565 $ 298.18
100.0 %
The following table provides the details of our medical claims
and benefits payable as of the dates indicated:
June 30, December 31,
2016 2015 Fee-for-service claims incurred but not
paid (IBNP) $ 1,292 $ 1,191 Pharmacy payable 103 88 Capitation
payable 37 140 Other (1) 334 266 $ 1,766 $ 1,685
(1) “Other” medical claims and
benefits payable include amounts payable to certain providers for
which we act as an intermediary on behalf of various state agencies
without assuming financial risk. Such receipts and payments do not
impact our consolidated statements of income. As of June 30, 2016
and December 31, 2015, we had recorded non-risk provider
payables of approximately $191 million and $167 million,
respectively.
MOLINA HEALTHCARE, INC.UNAUDITED
CHANGE IN MEDICAL CLAIMS AND BENEFITS PAYABLE(Dollars in
millions, except per-member amounts)
Our claims liability includes a provision for adverse claims
deviation based on historical experience and other factors
including, but not limited to, variations in claims payment
patterns, changes in utilization and cost trends, known outbreaks
of disease, and large claims. Our reserving methodology is
consistently applied across all periods presented. The amounts
displayed for “Components of medical care costs related to: Prior
period” represent the amount by which our original estimate of
claims and benefits payable at the beginning of the period were
more than the actual amount of the liability based on information
(principally the payment of claims) developed since that liability
was first reported. The following table presents the components of
the change in medical claims and benefits payable for the periods
indicated:
Year Ended Six Months Ended
June 30, December 31, 2016
2015 2015 Medical claims and benefits payable,
beginning balance $ 1,685 $ 1,201 $ 1,201 Components of medical
care costs related to: Current period 7,371 5,703 11,935 Prior
period (189 ) (138 ) (141 ) Total medical care costs 7,182
5,565 11,794 Change in non-risk provider
payables 24 14 48 Payments for medical care
costs related to: Current period 5,885 4,449 10,448 Prior period
1,240 839 910 Total paid 7,125 5,288
11,358 Medical claims and benefits payable, ending
balance $ 1,766 $ 1,492 $ 1,685 Benefit
from prior period as a percentage of: Balance at beginning of
period 11.3 % 11.5 % 11.8 % Premium revenue, trailing twelve months
1.3 % 1.2 % 1.1 % Medical care costs, trailing twelve months 1.4 %
1.4 % 1.2 % Fee-For-Service Claims Data: Days in claims
payable, fee for service 48 49 48 Number of members at end of
period 4,233,000 3,352,000 3,533,000 Number of claims in inventory
at end of period 530,900 463,200 380,800 Billed charges of claims
in inventory at end of period $ 1,279 $ 905 $ 816 Claims in
inventory per member at end of period 0.13 0.14 0.11 Billed charges
of claims in inventory per member at end of period $ 302.06 $
269.93 $ 230.91 Number of claims received during the period
26,279,000 18,679,000 40,173,300 Billed charges of claims received
during the period $ 31,649 $ 21,505 $ 46,211
View source
version on businesswire.com: http://www.businesswire.com/news/home/20160727006389/en/
Molina Healthcare, Inc.Investor Relations:Juan José Orellana,
562-435-3666, ext. 111143
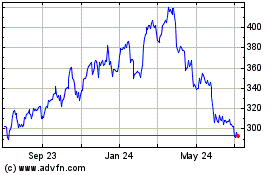
Molina Healthcare (NYSE:MOH)
Historical Stock Chart
From Mar 2024 to Apr 2024
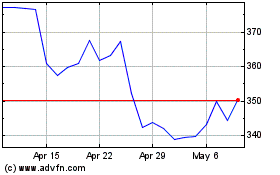
Molina Healthcare (NYSE:MOH)
Historical Stock Chart
From Apr 2023 to Apr 2024