UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 8-K
Current Report
Pursuant
to Section 13 or 15(d)
of the Securities Exchange Act of 1934
Date of Report (Date of earliest event reported): September 17, 2015
MOLINA HEALTHCARE, INC.
(Exact name of registrant as specified in its charter)
|
|
|
|
|
| Delaware |
|
1-31719 |
|
13-4204626 |
| (State of incorporation) |
|
(Commission
File Number) |
|
(I.R.S. Employer
Identification Number) |
200 Oceangate, Suite 100, Long Beach, California 90802
(Address of principal executive offices)
Registrant’s telephone number, including area code: (562) 435-3666
Check the appropriate box below if the Form 8-K filing is intended to simultaneously satisfy the filing obligation of the registrant under any of the
following provisions:
| |
¨ |
Written communications pursuant to Rule 425 under the Securities Act (17 CFR 230.425) |
| |
¨ |
Soliciting material pursuant to Rule 14a-12 under the Exchange Act (17 CFR 240.14a-12) |
| |
¨ |
Pre-commencement communications pursuant to Rule 14d-2(b) under the Exchange Act (17 CFR 240.14d-2(b)) |
| |
¨ |
Pre-commencement communications pursuant to Rule 13e-4(c) under the Exchange Act (17 CFR 240.13e-4(c)) |
| Item 7.01. |
Regulation FD Disclosure. |
On September 17, 2015, the Company presented and webcast certain slides
as part of the Company’s presentation at its Investor Day Conference held in New York City. A copy of the Company’s complete slide presentation is included as Exhibit 99.1 to this report. An audio and slide replay of the live
webcast of the Company’s Investor Day presentation will be available for 30 days from the date of the presentation at the Company’s website, www.molinahealthcare.com, or at www.earnings.com. The information contained in such websites is
not part of this current report.
The information in this Form 8-K current report and the exhibits attached hereto shall not be deemed to be
“filed” for purposes of Section 18 of the Securities Exchange Act of 1934 or otherwise subject to the liabilities of that section, nor shall it be deemed incorporated by reference in any filing under the Securities Act of 1933 or the
Securities Exchange Act of 1934, except as expressly set forth by specific reference in such a filing.
| Item 9.01. |
Financial Statements and Exhibits. |
(d) Exhibits:
|
|
|
Exhibit
No. |
|
Description |
|
|
| 99.1 |
|
Slide presentation given at the Investor Day Conference of Molina Healthcare, Inc. on September 17, 2015. |
SIGNATURE
Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by
the undersigned hereunto duly authorized.
|
|
|
|
|
|
|
MOLINA HEALTHCARE, INC. |
|
|
|
| Date: September 17, 2015 |
|
By: |
|
/s/ Jeff D. Barlow |
|
|
|
|
Jeff D. Barlow Chief Legal Officer and
Secretary |
EXHIBIT INDEX
|
|
|
| Exhibit
No. |
|
Description |
|
|
| 99.1 |
|
Slide presentation given at the Investor Day Conference of Molina Healthcare, Inc. on September 17, 2015. |
Exhibit 99.1
Cautionary Statement
Safe Harbor Statement under
the Private Securities Litigation Reform Act of 1995:This slide presentation and our accompanying oral remarks contain numerous “forward-looking statements” regarding, without limitation: our growth and acquisition expectations and
strategies; the closing of our announced acquisitions, the success of our integration efforts, and the projected revenues and profitability of our acquisitions; our ongoing margin improvement efforts; dual demonstration program growth and program
extensions; financial reconciliations under our various government contracts; the reimbursement of the ACA health insurer fee; our projected earnings for the second half of 2015; our longer-term financial objectives; expected rate changes; the
continuation of our Puerto Rico contract; and various other matters. All of our forward-looking statements are subject to numerous risks, uncertainties, and other factors that could cause our actual results to differ materially. Anyone viewing or
listening to this presentation is urged to read the risk factors and cautionary statements found under Item 1A in our annual report on Form 10-K, as well as the risk factors and cautionary statements in our quarterly reports and in our other
reports and filings with the Securities and Exchange Commission and available for viewing on its website at www.sec.gov.Except to the extent otherwise required by federal securities laws, we do not undertake to address or update forward-looking
statements in future filings or communications regarding our business or operating results.
© 2015 MOLINA
HEALTHCARE, INC.
2

Investor day 2015B
Agenda
Approx. Time Topic Speaker
12:30pm-12:35pm Opening Remarks Juan José Orellana, SVP Investor Relations
12:35pm-1:20pm Business Overview J. Mario Molina, MD, Chief Executive Officer
1:20pm-1:35pm Operations Review Terry Bayer, Chief Operating Officer
1:35pm-1:55pm Q&A
1:55pm-2:15pm Break
2:15pm-2:45pm Accounting Review Joseph White, Chief Accounting Officer
2:45pm-3:30pm Acquisition and Margin Improvement Review John Molina, Chief Financial Officer
3:30pm-3:50pm Q&A
3:50pm End of Program
© 2015 MOLINA
HEALTHCARE, INC.
3
Key investor inquiries
How will Molina continue
to grow? What’s changing in our space? Why Providence Human Services? What else is expected in 2015?
What
progress is being made in improving margins?
© 2015 MOLINA HEALTHCARE, INC.
4
J. Mario Molina M.D.
President & Chief
Executive Officer
5
Our mission
To provide quality health care to
people receiving government assistance
© 2015 MOLINA HEALTHCARE, INC.
6
Our footprint today
Health plan footprint
includes 4 of 5 largest Medicaid markets
1. Total enrollment relates to effective membership as of
June 30, 2015
© 2015 MOLINA HEALTHCARE, INC.
Puerto Rico
Molina Health plans Molina Medicaid Solutions Direct delivery
1
3.4M
Members
1% Duals
1% Medicare
8% Marketplace
USVI
11% ABD
14% Expansion
65% TANF & CHIP
Member Mix
7
Growth
While growth in the Medicaid program was
significant between 2013-2015, steady organic growth is expected over the next five years.
85M
136kMedicaid/CHIP Growth Projections1
82.2M
80.8M 81.5M
80M 79.8M 53k
77.9M
76.3M 21k 66k
75M 135k
72.1M 64k
70M
65M
2013 2014 2015 2016 2017 2018 2019 2020
1. CMS, Office of the Actuary, National Health Expenditure Projections 2014—2024, Table 17 Health
Insurance Enrollment and Enrollment Growth Rates https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsProjected.html
2. Enrollment as of June 30, 2015
© 2015 MOLINA HEALTHCARE, INC.
Year to Date
Enrollment Growth
December31, 2014
2.6M
members
Investor Day 2015B (today)
3.4M2
members
8
Where will our growth come from?
Organic growth
in existing markets and RFPs In-market acquisitions Marketplace Transition of members and benefits from FFS to managed care Capability-based provider acquisitions
© 2015 MOLINA HEALTHCARE, INC.
9
Continued organic growth in Medicare-Medicaid Plans (MMP)
Dual eligible markets
California Illinois USVI
Michigan Ohio South Carolina2
Puerto Rico
Texas
Total
Enrollment
December August 2014 20151 11K 15K
5K 4K
- 8K
2K 10K
- <1K
- 15K
18K 53K
MMP Markets
1. CMS enrollment data as of August,
2015
2. Voluntary enrollment only as of August, 2015
© 2015 MOLINA HEALTHCARE, INC.
10
In-market health plan acquisitions
State:
Illinois
Enrollment: 60,000
Annualized Revenue: $200M
State: Michigan
Enrollment: 85,000
Annualized Revenue: $270M
State: Florida
Enrollment: 62,000
Annualized Revenue: $200M
State: Florida
Enrollment: 25,000 Annualized Revenue: $80M
State: Florida
Enrollment: 90,000
Annualized Revenue: $250M
Generally asset purchases
Provide additional scale in existing areas
Increase access into new service areas
Accretive
Approximately $1.0B total annualized
revenue
Note: Estimated revenue based on annualized Company estimates
© 2015 MOLINA HEALTHCARE, INC.
11
Marketplace
15M
Penalty for not having coverage in 2016 is 2.5% of yearly household income or $695 per adult (half for those under 18)
USVI
Puerto Rico
Marketplace operations
230K1
Molina Marketplace Enrollment
18K
2Q2014 Aug 2015
93% of Molina marketplace members receive government subsidies
1. Company’s approximate enrollment as of August, 2015
© 2015 MOLINA HEALTHCARE, INC.
12
Increasing complexity drives higher spend
Complex
members continue to transition into managed care
Number of potential enrollees
$ $
Long Term Care
Dual Eligible $
Seniors & Persons $ with Disabilities
Medicaid Expansion
Temporary Assistance to Needy
Families
© 2015 MOLINA HEALTHCARE, INC.
13
Fee for service remains significant
Managed care
organizations and fee for service FY 2011
57M $404B
Fee-For-Service 15M 26% $307B 76%
Managed Care 42M 74%
$97B
24%
Medicaid Enrollment 2011
Medicaid Benefit
Spending 2011
76%
of Medicaid spending remains in Fee-for-Service
Sources:
1. Medicaid and CHIP Payment and Access Commission; Report to the Congress on Medicaid and CHIP; June 2014
2. CMS Medicaid Managed Care Enrollment Report, Summary Statistics as of July 1, 2011; June 1, 2012
© 2015 MOLINA HEALTHCARE, INC.
14
Medicaid Long Term Services and Supports (LTSS)
LTSS is a significant portion of fee for service spend
6%
People with Serious Mental Illness
30%
People with Developmental Disabilities
3%
Other/Multiple Populations
61%
Older People & People with Physical Disabilities
Full Medicaid LTSS Spend in 2012: $140 Billion1
1. Truven Health Analytics. ‘Medicaid Expenditures for Long-Term Services and Supports in FFY 2012; published April 28, 2014.
© 2015 MOLINA HEALTHCARE, INC.
15
Home and Community Based Services
Behavioral and
mental health services are significant drivers of cost
Medicaid HCBS Expenditures
FY 20101
Prevocational services
Day habilitation
Education services
Day treatment/partial hospitalization
Adult day
health
Adult day services
Community integration
Medical day care for
children
Home-based habilitation
Home health aide
Personal care
Companion
Homemaker
Chores
Group living, mental health services Round-the-clock services, unspecified Group living, other Shared living, other
In-home residential habilitation In-home round-the-clock services, other Group living, residential habilitation Shared living, residential habilitation In-home round-the-clock mental health services
Other2
14%
Day Services
15%
Home-Based
18%
Round-the-clock
46%
Mental Health
3%
Case Management
4%
Medicaid HCBS total spend in 2012: $69B
1. Mathematica Policy Research. ‘The HCBS Taxonomy: A New Language for Classifying Home- and Community-Based Services’, August 2013.
2. Other includes expenses related to goods and services, interpreters, housing consultation, and claims where the
procedure code could not be interpreted.
© 2015 MOLINA HEALTHCARE, INC.
16
Molina – changes in spend
Select Categories
2012 vs. 20151
$500M $465M
2012
$400M 2015E
$335M $330M
$300M
$200M
$160M
$110M
$100M $80M
$0M
Specialty Rx Personal Attendant 2 Behavioral Health
Services
1. 2015 estimates are based on full year annualized results as extrapolated from the results through the first half of 2015
2. Excludes amounts paid by state Medicaid agencies on Molina’s behalf
© 2015 MOLINA HEALTHCARE, INC.
17
Capability-based provider acquisitions – changes in delivery
5
Increasing Role of Data & Technology
1
Importance of the Member
Vertical Integration
& Broader
4
Continuum of Care
Member Centric Approach
Increasing Role of Government as a Payor 2
Value-Based Reimbursement
3
© 2015 MOLINA HEALTHCARE, INC.
1 Importance of the Member
Member will pay a larger portion of medical costs through Member-Directed / High Deductible Health Plans and Health Insurance Exchanges, and will demand increased choice and access to
care, more information regarding price, treatment options and information technology
2 Increasing Role of
Government as a Payor
Medicare, Medicaid and Exchanges represent the fastest growth areas
3 Value-Based Reimbursement
Shifting from Fee-For-Service to risk-based capitation and bundled payments, increasing role of Accountable Care Organizations (ACOs)
4 Vertical Integration & Broader Continuum of Care
Ownership of provider/care delivery assets to better manage care and medical costs, and capture “care margin”
5 Increasing Role of Data & Technology
HCIT is critical to the measurement and management of medical cost and engagement with the patient
18
Capability-based provider acquisition – behavioral health
Providence Human Services1, a multi-state, behavioral/mental health and social services provider
Operations in 23 states + DC? Medicaid focus:
80%
of revenue
Approximately 70% of all contracts are FFS
Diverse revenue base:
~100 contracts represent 70% of total revenue
More than 6,800 employees
Consideration ~ $200M2
1. The PHS transaction was
announced on September 3, 2015 and is subject to regulatory approvals and the satisfaction of other closing conditions
2. Subject to customary working capital and adjustments
© 2015 MOLINA HEALTHCARE, INC.
19
Diagnoses of behavioral and mental health conditions are increasing
Mental and substance use disorders are expected to surpass all physical diseases as a major cause of worldwide disability by 2020
Prevalence of mental illness among the Medicaid population is twice that of the general population
2X-3X
Treatment of chronic physical health issues for patients with behavioral health needs is 2 to 3 times more expensive than patients with physical health only needs.
68% of adults with mental illness also have at least 1 chronic physical illness.
49% of Medicaid enrollees with disabilities have a psychiatric illness.
Source: Annals of Internal Medicine: Crowley RA, Kirschner N, for the Health and Public Policy Committee of the American
College of Physicians. The Integration of Care for Mental Health, Substance Abuse, and Other Behavioral Health Conditions into Primary Care: Executive Summary of an American College of Physicians Position Paper. Ann Intern Med. 2015;163:298-299.
doi:10.7326/M15-0510
© 2015 MOLINA HEALTHCARE, INC.
20
Molina members with complex conditions
Top
diagnoses by segment by number of admits/cases trailing 12 months1
TANF Diagnoses ABD Diagnoses Dual Eligibles
Diagnoses
Inpatient Services
Delivery Septicemia Septicemia
Complications of
delivery Schizophrenic disorders Care involving use of rehabilitation procedures
Other maternal complications
Affective psychoses Schizophrenic disorders
Prolonged pregnancy Other diseases of lung Pneumonia
Affective psychoses Chronic bronchitis Diabetes
Outpatient Services
Well Child care Renal failure
Renal failure
Acute upper respiratory infection Schizophrenic disorders Schizophrenic disorders
Normal Pregnancy Hypertension Affective psychoses
Other maternal complications Diabetes Diabetes
General symptoms Affective psychoses Hypertension
1. Based on Company data ending June 30, 2015
© 2015 MOLINA HEALTHCARE, INC.
21
PHS – Adaptable contracting options
Different regulations/reimbursement policies dictate which services are offered in a particular geography
Medicaid Agency
Direct Behavioral Managed Care County Office or Behavioral Health Health Specialty Providers Local Organization Specialty Provider Provider
Indirect/Subcontracted Behavioral Health Specialty Provider
© 2015 MOLINA HEALTHCARE, INC.
22
What services does PHS provide?
More than 80% of
revenues are related to services focused on Mental Health1
Other2 10%
Autism & Intellectual and Developmental Disabilities 9%
Child Welfare 11%
Mental Health Child 44%
Mental Health Adult 26%
1. Based on Net Adjusted Revenues through 2014
2. Other includes Educational, Probational, and Substance Abuse
© 2015 MOLINA HEALTHCARE, INC.
23
Autism spectrum disorders (ASD) and Medicaid
1 in
68
children has been diagnosed with ASD1
72% of Medicaid recipients with ASD had at least 1 additional diagnosis2
CMS advised ASD treatment is considered covered under EPSDT benefits, not just waiver based (2014)3
1. US Centers for Disease Control and Prevention. http://www.cdc.gov/ncbddd/autism/data.html
2. Milliman Medicaid Issues Briefing Paper . http://us.milliman.com/uploadedFiles/insight/2015/expansion-asd-treatment.pdf
3. Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) program. CMS CMCS Information Bulletin,
July 7, 2014. http://www.medicaid.gov/Federal-Policy-Guidance/Downloads/CIB-07-07-14.pdf
© 2015
MOLINA HEALTHCARE, INC.
Increasingly being included in new state RFPs and Federal Regulations.
2013 Virginia Medicaid
Puerto Rico? Care coordination
2015 Washington
Foster Care
Care coordination
2015 Iowa Medicaid
2015 Wisconsin rate build
24
A growing need in Medicaid
The Medicaid program
finances more than one-quarter of the nation’s spending for behavioral health care and it is, by far, the largest single source of funding for public mental health services.
Source: Kaiser Family Foundation. Integrating Physical and Behavioral Health Care: Promising Medicaid Models. Feb 2014.
© 2015 MOLINA HEALTHCARE, INC.
25
An essential benefit
The ACA specifically
includes mental health and substance use disorder services as one of the ten categories of required “essential health benefits,” and the law requires parity between the mental and physical health benefits covered by health plans.
Source: Kaiser Family Foundation. Integrating Physical and Behavioral Health Care: Promising Medicaid Models.
Feb 2014.
26
© 2015 MOLINA HEALTHCARE, INC.
Integration
Nationwide, many state agencies,
health plans and providers are implementing PH/BH integration strategies in Medicaid.
27
© 2015 MOLINA HEALTHCARE, INC.
A strategic focus identifies greater needs
The
strategic focus leading to Molina’s growth in ABD, Dual Eligible and Long Term Care members is contributing to a higher spend in behavioral/mental heath services.
28
© 2015 MOLINA HEALTHCARE, INC.
A new provider capability
PHS revenue is
generated by 5,700 client-facing social workers, behavioral/mental health workers, case managers, licensed clinicians, psychologists, nurses and psychiatrists.
29
© 2015 MOLINA HEALTHCARE, INC.
Providence acquisition pro-forma footprint
Molina
will have a presence in 28 states 2 Commonwealths + Washington D.C.
Please refer to the Company’s
cautionary statement on page 2 of this presentation
Today
Molina Health plans
Molina Medicaid Solutions
Primary Care Direct
delivery
Virgin Islands
Puerto Rico
1. Behavioral/Mental health and
social services capabilities added through the acquisition of Providence Human Services (PHS) and Providence Community Services (PCS), with an anticipated closing in 4Q2015, pending regulatory approvals and the satisfaction of other closing
conditions.
Post Close
Molina Health plans
Molina Medicaid Solutions
Providence Human Services1
Pimary Care Direct delivery
Virgin Islands
Puerto Rico
30
© 2015 MOLINA HEALTHCARE, INC.
One of a kind
Flexible health services portfolio
(health plans, direct delivery, MMIS)
Focused on people receiving government assistance
Scalable administrative infrastructure
Consistent national brand
Seasoned management
team
Unique culture
31
© 2015 MOLINA HEALTHCARE, INC.
2015B
Investor Day
Terry Bayer
Chief Operating Officer
September 17, 2015 /
New York, New York
Medicare-Medicaid Plans (MMP)
Dual eligible
markets
USVI
Puerto Rico
MMP Markets
Enrollment
December August
2014 20151
California 11K 15K
Illinois 5K 4K
Michigan — 8K
Ohio 2K 10K
South Carolina2 — <1K
Texas — 15K
Total 18K 53K
1. CMS enrollment data as of August, 2015
2.
Voluntary enrollment only as of August, 2015
33
© 2015 MOLINA HEALTHCARE, INC.
Medicare – Dual Eligible Special Needs Plan
Our DSNP enrollment extends our dual eligible reach beyond just the Medicare Medicaid Plans
1
40K
members
USVI
Puerto Rico
Molina DSNP operations
1. CMS enrollment data as of August, 2015
34
© 2015 MOLINA HEALTHCARE, INC.
What’s new with the duals
All 6 Molina demos
have gone live nationally
2 year extension
From CMS for existing dual demonstration programs. All 6 of Molina’s states submitted letters of intent before the
September 1st deadline
CA, IL, OH extended until December 2019
MI, SC, TX extended until December 2020
Opportunities for continued growth
Age-ins
Part D re-assignees
Other passive enrollment opportunities at the state level
Retention
Reaching out to members that have opted
out resulted in more than 2K members returning to Molina.
More than 7K dual members enrolled voluntarily, and
have a 50% lower rate of disenrollment.
35
© 2015 MOLINA HEALTHCARE, INC.
Marketplace
15M
Penalty for not having coverage in 2016 is 2.5% of yearly household income or $695 per adult (half for those under 18)
Health Insurance Marketplace
1
230K
members
USVI
Puerto Rico
Marketplace operations
81% of our Marketplace revenue is in the form of subsidies
Nationally 84% of Marketplace enrollees receive the advanced premium tax credit subsidys2
75% of Molina
Marketplace membership are in a
silver plan
93% of Molina marketplace members receive government subsidies
1. Company’s approximate enrollment as of August, 2015
2. CMS June 30, 2015 Effectuated Enrollment Snapshot, released September 8, 2015;
https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-09-08.html
36
© 2015 MOLINA HEALTHCARE, INC.
Marketplace – staying true to the strategy
Priority segment: 100%-250% FPL
Medicaid transitioners; parents of CHIP members; ex-Medicaid members; low-income uninsured
Heavily subsidized
Used to getting care from
safety net providers
Require enhanced services
100%-250% FPL
Annual income levels for individuals $12K-$29K
250%-400% FPL
Annual income levels for individuals $29K-$47K
Ensuring continuity of care to those transitioning from Medicaid
37
© 2015 MOLINA HEALTHCARE, INC.
Marketplace – staying true to the strategy
Example: CA Minimum Wage
$9.00per hour
$18,720annualized
Premium assistance for marketplace is calculated based on the federal poverty scale. Individuals who earn <138% of the
FPL qualify for Medicaid.
FEDERAL POVERTY LEVELS & INCOME1,2
Size of 133% 138% 150% 200% 250%
Household
1 $ 15,654 $ 16,243 $ 17,655 $ 23,540 $
29,425
2 $ 21,187 $ 21,983 $ 23,895 $ 31,860 $ 39,825
3 $ 26,720 $ 27,724 $ 30,135 $ 40,180 $ 50,225
4 $ 32,253 $ 33,465 $ 36,375 $ 48,500 $ 60,625
5
$ 37,785 $ 39,206 $ 42,615 $ 56,820 $ 71,025
Hourly rate Hourly rate
$12.85 $14.49
Small hourly rate increases can affect Medicaid eligibility and marketplace subsidies
1. Office of the Assistant Secretary for Planning and Evaluation, http://aspe.hhs.gov/2015-poverty-guidelines
2. All dollar amounts are for the 48 contiguous states and DC
38
© 2015 MOLINA HEALTHCARE, INC.
Puerto Rico
Molina was awarded Medicaid contracts
in two regions in late 2014
San Juan
Caguas
Ponce
Southwest
East
Commenced operations on April 1, 2015
361,000 members as of 2Q2015 Estimated annualized revenue of $750M
Commonwealth continues to pay us weekly and
is current
39
© 2015 MOLINA HEALTHCARE, INC.
Q&A
40
2015B
Investor Day
Joseph White
Chief Accounting Officer
September 17, 2015
/ New York, New York
2015 income statement (unaudited)
Please refer to
the Company’s cautionary statement on page 2 of this presentation
Dollars (in millions)
YTD June 2015 FY 2015 Remaining
Actual Outlook1 Outlook2
Premium Revenue $6.3B
$13.5B $7.2B
Health Insurer Fee Revenue $122M $260M $138M
Premium Tax Revenue $190M $400M $210M
Service Revenue $99M $180M $81M
Investment and
Other Income $10M $17M $7M
Total Revenue $6.7B $14.3B $7.6B
Total Medical Care Cost $5.6B $12.1B $6.5B
Medical Care Ratio3 88.7% 89.5% n/a
Total Cost of
Service Revenue $69M $145M $76M
General & Administrative Expenses $0.5B $1.1B $0.6B
G&A Ratio4 8.1% 7.6% n/a
Premium Tax Expense $190M $400M $210M
Health
Insurer Fee Expense $81M $165M $84M
Depreciation & Amortization $50M $105M $55M
Interest & Other Expense $30M $60M $30M
Income before Taxes $168M $300M $132M
Net Income
$67M $132M $65M
EBITDA5 $256M $485M $229M
Effective Tax Rate 60.1% 56.0% n/a
Net Income Per Diluted Share $1.29 $2.35 $1.06
Adjusted Net Income Per Diluted Share5 $1.57 $2.90 $1.33
Amounts are estimates – actual results may differ materially. See our risk factors as discussed in our Form 10-K and
other periodic filings
1. Reflects fiscal year 2015 outlook as provided on June 1, 2015
2. Remaining outlook is the result of FYI 2015 outlook less YTD June 2015 actual only
3. Medical Care Ratio represents medical care costs as a percent of premium revenue
4. G&A ratio computed as a percentage of total revenue
5. See reconciliation of unaudited non-GAAP financial measures
42
© 2015 MOLINA HEALTHCARE, INC.

Reconciliation of non-GAAP financial measures
EBITDA and adjusted net income
Please refer to the Company’s cautionary statement on page 2 of this presentation.
EBITDA YTD June 2015 FY 2015 Remaining
Actual
Outlook1 Outlook2
Net income $67M $132M $65M
Adjustments:
Depreciation, and amortization of intangible assets and capitalized software $58M $125M $67M
Interest expense $30M $60M $30M
Income tax
expense $101M $168M $67M
EBITDA $256M $485M $229M
Adjusted net income per diluted share YTD June 2015 FY 2015 Remaining
Actual Outlook Outlook
Net income per diluted share $1.29 $2.35 $1.06
Adjustments, net of tax:
Amortization of convertible senior notes and lease financing obligations $0.18 $0.35 $0.17
Amortization of intangible assets $0.10 $0.20 $0.10
Adjusted net income per diluted share $1.57 $2.90 $1.33
Amounts are estimates – actual results may differ materially. See our risk factors as discussed in our Form 10-K and
other periodic filings
1. Reflects fiscal year 2015 outlook as provided on June 1, 2015
2. Remaining outlook is the result of FYI 2015 outlook less YTD June 2015 actual only
© 2015 MOLINA HEALTHCARE, INC.
43
Uncertainties relating to 2nd half earnings
Please refer to the Company’s cautionary statement on page 2 of this presentation
Issues State
MCR floor reconciliation CA, NM, WA
Cost plus
reconciliation NM
Quality revenue TX
HIF reimbursement MI
PR / MI MMP/ TX MMP /
MCR
Acquisitions / FL Rates
44
© 2015 MOLINA HEALTHCARE, INC.
Profit restrictions are significant
85% of
Premium revenue earned YTD 6/30/2015 is subject to profit restrictions
Marketplace, 6%
MMP, 7%
Medicaid Expansion, 17%
Medicare SNP, 4%
Medicaid no restrictions, 15%
Medicaid with restrictions, 51%
% of revenue
subject to
profit restrictions:
Medicaid: 75%
Medicaid Expansion: 100%
MMP Duals: 100%
Marketplace: 100%
Medicare SNP: 100%
45
© 2015 MOLINA HEALTHCARE, INC.
Payables due to profit restrictions
Please refer
to the Company’s cautionary statement on page 2 of this presentation
Dec-14 Jun-15
Medicaid Expansion:
California ~$120M ~$130M
New Mexico ~$25M ~$50M
Washington ~$240M ~$270M
Others — ~$15M
Medicaid Expansion Subtotal
~$385M ~$465M
Marketplace — ~$40M
Others ~$15M ~$35M
Total ~$400M ~$540M
46
© 2015 MOLINA HEALTHCARE, INC.
Marketplace medical care ratio
How do we report a
Marketplace MCR <80%
Six Months Ended June 30, 2015(1)
Premium Revenue Medical Care Costs
Member
Months(2) Total PMPM Total PMPM MCR(3)
Medical Margin
TANF and CHIP 12,035 $ 2,141,316 $177.93 $ 1,960,315 $162.89 91.5% $ 181,001
Medicaid Expansion 2,661 1,089,339 409.29 867,229 325.84 79.6 222,110
ABD 2,120 1,993,366 940.23 1,809,613 853.56 90.8 183,753
Marketplace 1,371 354,725 258.66 245,682 179.15 69.3 109,043
Medicare 264 273,472 1,036.95 269,005 1,020.01 98.4 4,467
MMP 213 422,806 1,986.04 413,474 1,942.20 97.8 9,332
18,664 $ 6,275,024 $336.21 $ 5,565,318 $298.18 88.7% $ 709,706
(1) Six months ended June 30, 2014 data not presented due to lack of comparability.
(2) A member month is defined as the aggregate of each month’s ending membership for the period presented.
(3) “MCR” represents medical costs as a percentage of premium revenue.
Molina healthcare 10-Q June 30, 2015
47
© 2015 MOLINA HEALTHCARE, INC.
Different calculations of Marketplace MCR
MOH
GAAP MCR
MOH 10K MCR
Medical Care Cost
MCR =
Premium Revenue
Min MCR Calculation
Federal Register Vol 78
No. 47; Monday March 11,
2013, Part II, HHS Notice of Benefit and Payment
Parameters for 2014, Page 15,505
MCR= [(i + q – s + n – r)/ {(p + s – n + r) – t – f – (s – n + r)}] + c
i = incurred claims
q = expenditures on quality
improving activities
p = earned premiums
t = Federal and State taxes and assessments
f = licensing and regulatory fees, including transitional reinsurance contributions
s = issuer’s transitional reinsurance receipts
n = issuer’s risk corridors and risk adjustment related payments
r=issuer’s risk corridors and risk adjustment related receipts
c = credibility adjustment, if any
48
© 2015 MOLINA HEALTHCARE, INC.
Marketplace example - GAAP vs. CMS minimum MCR
4%
(1%) 0%
1%
16%
80%
60%
1. GAAP MCR 2. Risk Adjustment / 3. QI Expenses 4. Taxes and Fees 5. Prior Year Adjustments 6. Credibilty Adjustments CMS MLR
Corridor and MLR Rebate
© 2015 MOLINA HEALTHCARE, INC.
49
Admin ratio – market place and profit restriction impact
Impact of lost revenue from profit restrictions
Impact of Marketplace fees
G&A ratio net of profit restrictions & Marketplace fees
12.0%
10.0%
8.0%
6.0%
4.0%
2.0%
0.0%
10.1%
10.0%
7.9%
7.5%
8.1%
7.2%
FY2013 FY2014 YTD-2Q15
50
© 2015 MOLINA HEALTHCARE, INC.
Diluted Shares outstanding 2015 (unaudited)
Please refer to the Company’s cautionary statement on page 2 of this presentation
70M
62M1 62M1
1M 1M
60M 56M1
54M
50M 56M 56M
50M
40M
30M
20M
10M
5M 6M
M
Q1 Q2 Q3 Q4 FY15
Other
Shares Outstanding
Convertible Note Dilution
Totals may not add due
to rounding
1. Q3, Q4 and FY 15 are estimates
© 2015 MOLINA HEALTHCARE, INC.
51
John C. Molina Chief Financial Officer
52
Acquisition strategy
How do the pieces fit
together
New Managed Care State Existing Managed Care State Provider / Capability
Rationale
Diversification – revenue, risk, contracts Fortify competitive position Enhance provider alignment
Administrative cost leverage – long term Administrative leverage – short term Medical cost improvement – medium term
Criteria
Increased member care oversite /
Competitive
provider environment Competitive provider environment
management
Sizeable Medicaid population Attractive price Complementary to Molina care model
Difficult /expensive / timely to develop
Favorable regulatory environment Favorable regulatory environment
internally
Valuable talent
© 2015 MOLINA HEALTHCARE, INC.
53
A closer look at our health plan acquisitions
Recent health plan M&A
Please refer to the Company’s cautionary statement on page 2 of this presentation
Transaction Status Membership1 Annualized Revenue1
MyCare Chicago Close pending 60,000 $200M
Integral Health Plan Close pending 90,000 $250M
HealthPlus Closed 85,000 $270M
Preferred Medical Plan Closed 25,000 $80M
Subtotal 260,000 $800M
1. Membership and annualized revenue reflect estimates as of the transaction announcement date for transaction that are pending close. For closed transactions membership reflects actual
members transferred to Molina and estimated revenues associated with those members.
© 2015 MOLINA
HEALTHCARE, INC.
54
Florida Medicaid footprint expansion
Recent
Florida acquisition summary1,2
Pensacola, Tampa & Sarasota service area served by
Integral Health Plan
December , 2015
90K members
Jacksonville service area served by
First Coast Advantage
December, 2014
62K members
Miami-Dade service area served by Molina and
Preferred Medical Plan
August, 2015
25K members
1. Transactions for Integral Health Plan & Preferred Medical have yet to close.
2. Enrollment numbers are estimates, based on the publically announced press release
© 2015 MOLINA HEALTHCARE, INC.
55
Capability-based provider acquisition – behavioral health
Providence Human Services1, a multi-state, behavioral/mental health and social services provider
Operations in 23 states + DC
Medicaid focus:
80% of revenue
Approximately 70% of all
contracts are FFS
Diverse revenue base:
~100 contracts represent 70%
of total revenue
More than 6,800 employees
Consideration ~ $200M2
1. The PHS transaction was
announced on September 3, 2015 and is subject to regulatory approvals and the satisfaction of other closing conditions
2. Subject to customary working capital and adjustments
© 2015 MOLINA HEALTHCARE, INC.
56
Providence Human Services strategic rationale
Why
Molina
Medicaid focus
Significantly advances our behavioral/mental health capabilities
Builds upon our direct delivery infrastructure
Creates market presence in new states relevant to these patients
Why PHS
Medicaid focus
A viable stand alone business that
brings new capabilities and overall margin improvement to our health plans
Large behavioral/mental health
provider with flexible model and adaptable services offering
Cross expansion opportunities to Molina
geographies
Cultural fit, mission and philosophy
2016+ FORTIFY
Consistent with our long term objectives of improving the model of care, enhancing our systems and improving our margins.
© 2015 MOLINA HEALTHCARE, INC.
57
PHS – Adaptable contracting options
Different regulations/reimbursement policies dictate which services are offered in a particular geography
Medicaid Agency
Direct Behavioral
Managed Care County Office or
Behavioral Health
Health Specialty
Providers Local Organization Specialty Provider
Provider
Indirect/Subcontracted Behavioral
Health
Specialty Provider
© 2015 MOLINA HEALTHCARE, INC.
58
What services does PHS provide
More than 80% of
revenues are related to services focused on Mental Health1
Mental Health
Other2 Child
10% 44%
Autism &
Intellectual and Mental Health
Developmental Adult
Disabilities 26%
9%
Child Welfare
11%
1. Based on Net Adjusted Revenues through 2014
2. Other includes Educational, Probational, and Substance Abuse
© 2015 MOLINA HEALTHCARE, INC.
59
PHS – net revenue breakdown by payor
Other1
7% Medicaid
Intermediaries
Medicaid (Government,
Direct State and
27% 35% US Agencies)
Medicaid
83% 21%
Insurance / HMO’s /
Other Health Plans
Medicaid Intermediaries
10% (Cities and Local Boards)
1. Other includes Educational, Probational, Workforce Development and Substance Abuse
© 2015 MOLINA HEALTHCARE, INC.
60
2015 and beyond
2013 2014 2015 2016+
INCUBATE TRANSITION & GROW DEVELOP & GROW FORTIFY
Acquire new business Transition members into model of Transition members into model of Improve model of care
Design systems care care Enhance systems
Test readiness Address pent-up demand Address pent-up demand Improve margins
Invest in infrastructure Adjust premiums Adjust premiums
New business: Process transition issues Improve systems
SC, Duals, Marketplace, Medicaid Begin leveraging infrastructure Ensure equitable rates
Expansion, NM & FL re- Invest to prepare for 2015 revenue Leverage administrative costs
procurements, WI Medicare
© 2015 MOLINA
HEALTHCARE, INC.
61
2017 Financial objectives
Please refer to the
Company’s cautionary statement on page 2 of this presentation
Revenue growth
~0.5%-1.5% decline in medical cost ratio ~0.5%—1.0% decline in G&A ratio Target: ~1.5%—2.0% after tax margin
How will we get there
Actuarially sound premium rates Manage inpatient costs Network alignment Retention of members
© 2015 MOLINA HEALTHCARE, INC.
62
Premium revenue
We expect 2016 premium revenue to
be at least $1.0B higher than in 2015
Please refer to the Company’s cautionary statement on page 2 of
this presentation
$14.6B
$13.5B
Full year 2015 Outlook December 2015 Run
Rate1
Both numbers are Company estimates
1. Month of December 2015 Annualized
© 2015 MOLINA HEALTHCARE, INC.
63
High cost member intervention
A look at dual
eligibles and ABDs
3%
30%
97%
70%
Members Medical Costs
3% of our dual eligible
members and 3% of our ABD members account for 30% of our medical costs under each line of business.
©
2015 MOLINA HEALTHCARE, INC.
64
Admin ratio – market place and profit restriction impact
Please refer to the Company’s cautionary statement on page 2 of this presentation
12.0%
10.1%
10.0%
7.9% 8.1%
8.0%
6.0%
10.0%
4.0% 49%
7.5% 7.2%
2.0%
0.0%
FY2013 FY2014 YTD-2Q15
Admin ratio sensitivity
Every $1 billion of
incremental revenue:
requires between $43 million and $50 million of new G&A spend
G&A ratio declines between 10 75% to 20 bps
40 bps decrease in G&A ratio increases after tax margins by 25 bps
Impact of Profit Restrictions on G&A Ratio
Impact of Marketplace Fees
G&A Ratio Net Profit Restrictions & Marketplace Fees
© 2015 MOLINA HEALTHCARE, INC.
65
Investment income
Interest rate sensitivity on
investment income
Please refer to the Company’s cautionary statement on page 2 of this presentation
Investment Income EPS
$35M $ 2.65
$30M $ 2.60
$25M
$ 2.55
$20M
$ 2.50
$15M
$ 2.45
$10M
$5M $ 2.40
$0M $ 2.35
0.50% 0.75% 1.00% 1.25% 1.50%
Increase in Fed Funds Rate
Investment Income EPS
Each 25bp increase in rates results in $5M to $6M more of annualized investment income
© 2015 MOLINA HEALTHCARE, INC.
66
Effective tax rate
ETR sensitivity to pretax
income1
Please refer to the Company’s cautionary statement on page 2 of this presentation
Growing pretax income mitigates the impact of non-deductible expenses, lowering the effective tax rate
100%
95%
90%
80%
70%
Tax Rate
60% 57%
50% 45%
40%
30%
$100M $200M $300M $400M $500M $600M $700M $800M
Pretax income
1. ETR includes estimated 2015 non deductible expenses
© 2015 MOLINA HEALTHCARE, INC.
67
After tax margin sensitivity
Each 25bps increase
in after tax margin increases EPS by $0.65
Please refer to the Company’s cautionary statement on page 2
of this presentation
$10.00
$8.00
$6.00
$5.10
EPS
$4.00 EPS
$2.35
$2.00
$0.00
0.0% 0.5% 1.0% 1.5% 2.0% 2.5% 3.0%
After Tax Margin
Based on 2015 Outlook
© 2015 MOLINA HEALTHCARE, INC.
68
After tax margin
Historical and outlook
Please refer to the Company’s cautionary statement on page 2 of this presentation
2.0%
2.0%
1.8%
1.6% 1.5%
1.4%
1.2%
1.0%
1.0%
0.8%
0.8%
0.6%
0.6%
0.4%
0.2%
0.0%
2013 2014 June 30, 2015 YTD 2016 2017 Long Term
Outlook
© 2015 MOLINA HEALTHCARE, INC.
69
Rate changes revisited
Please refer to the
Company’s cautionary statement on page 2 of this presentation
Baseline Outlook 1
State
Effective Date Rate Change
California Jul-15 +2%
Florida Sep-15 +4%
Illinois Jul-15 TBD
Michigan 8% Oct-15 TBD
LTC
New Mexico Jan-15 +3%
Ohio Jan-15 +1%
South Carolina Jul-15 (3%)
Texas Jul-153 /Sep-15 +3% /+2%
Utah Jan-154
/Jul-15 +3% / TBD
Washington 11% Jan-15 +3%
ABD
Wisconsin Jan-15 +0.5%
Medicaid Expansion
State
Effective Date Rate Change
California Jan-152
/Jul-15 (16%) / (12%)
Illinois Jul-15 TBD
Michigan Oct-15 TBD
New Mexico Jan-15 +4%
Ohio Jan-15 (3%)
Washington Jan-15/Jul-15 (41%) / (8%)
70
Q&A
71
Molina Healthcare (NYSE:MOH)
Historical Stock Chart
From Aug 2024 to Sep 2024
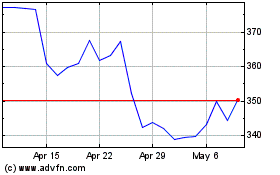
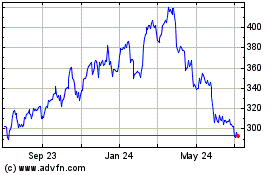
Molina Healthcare (NYSE:MOH)
Historical Stock Chart
From Sep 2023 to Sep 2024