Molina Healthcare, Inc. (NYSE: MOH):
- Net income per diluted share,
continuing operations, of $0.72 for the quarter, compared with
$0.16 in 2014.
- Adjusted net income per diluted share,
continuing operations,1 of $0.86 for the quarter, compared with
$0.32 for 2014.
- Total revenue of $3.5 billion, up 52%
over second quarter 2014 and 11% over first quarter 2015.
Molina Healthcare, Inc. (NYSE: MOH) today reported its financial
results for the second quarter of 2015.
“Our second quarter results mark continued progress and momentum
in our business. We were able to improve our profit margins
while simultaneously growing our top-line revenue and enrollment,”
said J. Mario Molina M.D., chief executive officer of Molina
Healthcare, Inc. “We remain confident that we have the right plans
in place for the rest of 2015 and look forward to closing our
recently announced Medicaid acquisitions in Florida, Illinois, and
Michigan later this year.”
Overview of Financial Results, Continuing Operations
Financial results for the second quarter of 2015 improved
significantly over the same quarter of 2014 due to higher revenue,
greater medical and administrative cost efficiency, and more
complete state reimbursement of the Affordable Care Act Health
Insurer Fee (HIF).
Income from continuing operations, before tax expense, increased
to $101 million in the second quarter of 2015, from $18 million in
the second quarter of 2014, and $67 million in the first quarter of
this year.
Premium revenue increased approximately 52% in the second
quarter of 2015 compared with the second quarter of 2014 due to
increased Medicaid expansion and Marketplace enrollment, growth in
the Company’s Illinois health plan, and the recent start-up of the
Company’s Puerto Rico health plan.
Medical care costs as a percent of premium revenue (the “medical
care ratio”) decreased to 88.7% in the second quarter of 2015, from
89.3% in the second quarter of 2014, and were unchanged from the
first quarter of this year.
General and administrative expenses as a percentage of total
revenue (the “general and administrative expense ratio”) decreased
to 8.1% in the second quarter of 2015, from 8.4% in the second
quarter of 2014, and were unchanged from the first quarter of this
year.
Financing Activities
In June 2015, the Company issued 5.75 million shares of common
stock, raising $373 million after offering costs. Additionally in
June 2015, the Company entered into a $250 million revolving credit
facility. Both of these actions will finance working capital needs,
acquisitions, capital expenditures, and other general corporate
activities.
Health Insurer Fee Update
The Company continues to make progress in securing full
reimbursement for the Medicaid portion of its expense under the
Affordable Care Act Health Insurer Fee (HIF).
During the second quarter of 2015, the Company recognized as
revenue the entire HIF reimbursement due from California for the
period January 1, 2014 through June 30, 2015. The Company
recognized approximately $12 million ($0.14 per diluted share)
related to 2014; and approximately $17 million ($0.20 per diluted
share) related to the first half of 2015. After allowing for HIF
revenue not recognized for Michigan and Utah (approximately $8
million, or $0.10 per diluted share, for each of the first and
second quarters), the net impact of HIF reimbursement was $12
million ($0.14 per diluted share) favorable for the second quarter
and $5 million ($0.06 per diluted share) unfavorable for the six
months ended June 30.
The comparable amount of HIF reimbursement not recognized in
2014 was approximately $15 million ($0.20 per diluted share) for
the second quarter and approximately $32 million ($0.42 per diluted
share) for the six months ended June 30.
Texas Health Plan Quality Revenue Update
As previously disclosed, the Company has deferred recognition of
that portion of its quality related revenue in Texas that is based
upon measures for which the Company does not have historical
information, clear definitions, and clarity around minimum
standards. Such revenue is estimated to be approximately $20
million for all of 2014 and $12 million for the first half of 2015.
The Company has not recognized any of this revenue through June 30,
2015.
Conference Call
The Company’s management will host a conference call and webcast
to discuss its second quarter results at 5:00 p.m. Eastern time on
Thursday, July 30, 2015. The number to call for the interactive
teleconference is (212) 231-2937. A telephonic replay of the
conference call will be available from 7:00 p.m. Eastern time on
Thursday, July 30, 2015, through 6:00 p.m. on Friday, July 31,
2015, by dialing (800) 633-8284 and entering confirmation number
21770257. A live audio broadcast of Molina Healthcare’s conference
call will be available on the Company’s website, molinahealthcare.com. A 30-day online replay will
be available approximately an hour following the conclusion of the
live broadcast.
About Molina Healthcare
Molina Healthcare, Inc., a FORTUNE 500 company, provides managed
health care services under the Medicaid and Medicare programs and
through the state insurance marketplaces. Through our locally
operated health plans in 11 states across the nation and in the
Commonwealth of Puerto Rico, Molina currently serves over 3 million
members. Dr. C. David Molina founded our company in 1980 as a
provider organization serving low-income families in Southern
California. Today, we continue his mission of providing high
quality and cost-effective health care to those who need it most.
For more information about Molina Healthcare, please visit our
website at molinahealthcare.com.
Notes:
1. Adjusted net income per diluted share, continuing operations,
is a non-GAAP financial measure used by management as a
supplemental metric in evaluating its financial performance, its
financing and business decisions, and in forecasting and planning
for future periods. This measure is not determined in accordance
with accounting principles generally accepted in the United States
of America (GAAP) and should not be viewed as a substitute for the
most directly comparable GAAP measure, which is diluted net income
per share, continuing operations. See below for reconciliations of
the Company’s non-GAAP measures to the most directly comparable
GAAP measures.
Safe Harbor Statement under the Private Securities Litigation
Reform Act of 1995: This earnings release contains
“forward-looking statements” regarding the Company’s plans,
expectations, and anticipated future events. Actual results could
differ materially due to numerous known and unknown risks and
uncertainties. Those known risks and uncertainties include, but are
not limited to the following:
- uncertainties associated with the
implementation of the Affordable Care Act, including the full
grossed up reimbursement by states of the non-deductible ACA health
insurer fee, the Medicaid expansion, the insurance marketplaces,
the effect of various implementing regulations, and uncertainties
regarding the Medicare-Medicaid dual eligible demonstration
programs in California, Illinois, Michigan, Ohio, South Carolina,
and Texas;
- management of our medical costs,
including seasonal flu patterns and rates of utilization that are
consistent with our expectations, and our ability to reduce over
time the high medical costs commonly associated with new patient
populations;
- federal or state medical cost
expenditure floors, administrative cost and profit ceilings, and
profit sharing arrangements;
- the interpretation and implementation
of at-risk premium rules regarding the achievement of certain
quality measures, including 2014 and 2015 at-risk premium rules in
the state of Texas;
- cyber-attacks or other privacy or data
security incidents resulting in an inadvertent unauthorized
disclosure of protected health information;
- the success of our new health plan in
Puerto Rico, including the successful resolution of the Puerto Rico
debt crisis and the payment of all amounts due under our Medicaid
contract;
- newly FDA-approved specialty drugs such
as Sovaldi, Olysio, Harvoni, and other specialty drugs or generic
drugs that are exorbitantly priced but not factored into the
calculation of our capitated rates;
- significant budget pressures on state
governments and their potential inability to maintain current
rates, to implement expected rate increases, or to maintain
existing benefit packages or membership eligibility thresholds or
criteria, including the resolution of the Illinois budget impasse
and continued payment of our Illinois health plan;
- the accurate estimation of incurred but
not paid medical costs across our health plans;
- retroactive adjustments to premium
revenue or accounting estimates which require adjustment based upon
subsequent developments, including Medicaid pharmaceutical rebates
or retroactive premium rate increases;
- efforts by states to recoup previously
paid amounts;
- the success of our efforts to retain
existing government contracts and to obtain new government
contracts in connection with state requests for proposals (RFPs) in
both existing and new states, including the pending Medicaid RFP in
Michigan;
- the continuation and renewal of the
government contracts of both our health plans and Molina Medicaid
Solutions and the terms under which such contracts are
renewed;
- complications, member confusion, or
enrollment backlogs related to the annual renewal of Medicaid
coverage;
- government audits and reviews, and any
fine, enrollment freeze, or monitoring program that may result
therefrom;
- changes with respect to our provider
contracts and the loss of providers;
- approval by state regulators of
dividends and distributions by our health plan subsidiaries;
- changes in funding under our contracts
as a result of regulatory changes, programmatic adjustments, or
other reforms;
- high dollar claims related to
catastrophic illness;
- the favorable or unfavorable resolution
of litigation, arbitration, or administrative proceedings,
including pending qui tam actions in California and Florida, and
the litigation commenced against us by the state of Louisiana
alleging that Molina Medicaid Solutions and its predecessors used
an incorrect reimbursement formula for the payment of
pharmaceutical claims;
- the relatively small number of states
in which we operate health plans;
- our management of a portion of College
Health Enterprises’ hospital in Long Beach, California;
- the availability of adequate financing
on acceptable terms to fund and capitalize our expansion and
growth, repay our outstanding indebtedness at maturity and meet our
liquidity needs, including the interest expense and other costs
associated with such financing;
- the failure of a state in which we
operate to renew its federal Medicaid waiver;
- changes generally affecting the managed
care or Medicaid management information systems industries;
- increases in government surcharges,
taxes, and assessments;
- public alarm associated with newly
emergent viruses or widespread epidemics;
- changes in general economic conditions,
including unemployment rates;
- increasing competition and
consolidation in the Medicaid industry;
and numerous other risk factors, including those discussed in
the Company’s periodic reports and filings with the Securities and
Exchange Commission. These reports can be accessed under the
investor relations tab of the Company’s website or on the SEC’s
website at sec.gov. Given these risks
and uncertainties, we can give no assurances that the Company’s
forward-looking statements will prove to be accurate, or that any
other results or events projected or contemplated by the Company’s
forward-looking statements will in fact occur, and we caution
investors not to place undue reliance on these statements. All
forward-looking statements in this release represent the Company’s
judgment as of July 30, 2015, and we disclaim any obligation to
update any forward-looking statements to conform the statement to
actual results or changes in the Company’s expectations.
MOLINA HEALTHCARE, INC.
UNAUDITED CONSOLIDATED STATEMENTS OF
INCOME
Three Months Ended
June 30,
Six Months Ended
June 30,
2015 2014 2015 2014
(Amounts in thousands, except net income per share) Revenue:
Premium revenue $ 3,304,372 $ 2,167,142 $ 6,275,024 $ 4,107,479
Service revenue 47,243 50,232 99,101 103,862 Premium tax revenue
94,609 70,120 189,956 121,813 Health insurer fee revenue 73,890
19,662 121,838 38,358 Investment income 3,828 1,945 6,843 3,574
Other revenue 948 2,938 3,251 6,196
Total revenue 3,524,890 2,312,039 6,696,013
4,381,282 Operating expenses: Medical care costs 2,929,534
1,934,299 5,565,318 3,655,957 Cost of service revenue 32,819 37,107
68,721 77,764 General and administrative expenses 286,496 193,239
542,586 381,326 Premium tax expenses 94,609 70,120 189,956 121,813
Health insurer fee expenses 40,652 21,945 81,430 44,135
Depreciation and amortization 25,152 22,902 50,144
43,593 Total operating expenses 3,409,262
2,279,612 6,498,155 4,324,588 Operating income
115,628 32,427 197,858 56,694 Other
expenses, net: Interest expense 14,946 13,993 29,822 27,815 Other
income, net (32 ) (9 ) (42 ) (53 ) Total other expenses, net 14,914
13,984 29,780 27,762
Income from continuing operations before
income tax expense
100,714 18,443 168,078 28,932 Income tax expense 61,783
10,702 101,006 16,357 Income from continuing
operations 38,931 7,741 67,072 12,575
Income (loss) from discontinued
operations, net of tax
12 70 24 (266 ) Net income $ 38,943 $
7,811 $ 67,096 $ 12,309 Diluted net
income per share: Income from continuing operations $ 0.72 $
0.16 $ 1.29 $ 0.26 Diluted net income per
share $ 0.72 $ 0.16 $ 1.29 $ 0.26
Diluted weighted average shares outstanding 53,871
48,003 52,008 47,824
Operating
Statistics, Continuing Operations: Medical care ratio (1) 88.7
% 89.3 % 88.7
%
89.0 % Service revenue ratio (2) 69.5 % 73.9 % 69.3 % 74.9 %
General and administrative expense ratio (3) 8.1 % 8.4 % 8.1 % 8.7
% Premium tax ratio (1) 2.8 % 3.1 % 2.9 % 2.9 % Effective tax rate
61.3 % 58.0 % 60.1 % 56.5 % Net profit margin, continuing
operations (3) 1.1 % 0.3 % 1.0 % 0.3 %
(1) Medical care ratio represents medical
care costs as a percentage of premium revenue; premium tax ratio
represents premium tax expenses as a percentage of premium revenue
plus premium tax revenue. Medical care costs include costs incurred
for providing long term services and supports (LTSS).
(2) Service revenue ratio represents cost
of service revenue as a percentage of service revenue.
(3) Computed as a percentage of total
revenue.
MOLINA HEALTHCARE, INC.
UNAUDITED CONSOLIDATED BALANCE
SHEETS
June 30, 2015
December 31,
2014
(Unaudited) (Amounts in thousands,except per-share
data) ASSETS Current assets: Cash and cash equivalents $
2,013,882 $ 1,539,063 Investments 1,466,622 1,019,462 Receivables
631,124 596,456 Deferred income taxes 37,480 39,532 Prepaid
expenses and other current assets 148,615 50,884 Derivative asset
508,504 — Total current assets 4,806,227 3,245,397
Property, equipment, and capitalized software, net 363,244 340,778
Deferred contract costs 65,410 53,675 Intangible assets, net 80,462
89,273 Goodwill 272,046 271,964 Restricted investments 110,956
102,479 Derivative asset — 329,323 Other assets 37,814
44,326 $ 5,736,159 $ 4,477,215
LIABILITIES AND STOCKHOLDERS’ EQUITY Current liabilities:
Medical claims and benefits payable $ 1,492,252 $ 1,200,522 Amounts
due government agencies 824,934 527,193 Accounts payable and
accrued liabilities 399,186 241,654 Deferred revenue 57,723 196,076
Income taxes payable 10,396 8,987 Current portion of long-term debt
445,668 341 Derivative liability 508,355 — Total
current liabilities 3,738,514 2,174,773 Convertible senior notes
272,930 704,097 Lease financing obligations 161,323 160,710 Lease
financing obligations - related party 40,016 40,241 Deferred income
taxes 29,174 24,271 Derivative liability — 329,194 Other long-term
liabilities 31,095 33,487 Total liabilities 4,273,052
3,466,773 Stockholders’ equity: Common stock, $0.001
par value; 150,000 shares authorized; outstanding: 56,050 shares at
June 30, 2015 and 49,727 shares at December 31, 2014 56 50
Preferred stock, $0.001 par value; 20,000 shares authorized, no
shares issued and outstanding — — Additional paid-in capital
782,433 396,059 Accumulated other comprehensive loss (1,830 )
(1,019 ) Retained earnings 682,448 615,352 Total
stockholders’ equity 1,463,107 1,010,442 $ 5,736,159
$ 4,477,215
MOLINA HEALTHCARE, INC.
UNAUDITED CONDENSED CONSOLIDATED
STATEMENTS OF CASH FLOWS,
CONTINUING AND DISCONTINUED
OPERATIONS
Three Months Ended June 30, Six Months Ended June
30, 2015 2014 2015
2014 (Amounts in thousands) Operating activities: Net
income $ 38,943 $ 7,811 $ 67,096 $ 12,309
Adjustments to reconcile net income to net
cash provided by operating activities:
Depreciation and amortization 29,502 32,660 62,076 65,654 Deferred
income taxes 6,308 2,362 7,405 1,692 Share-based compensation 3,566
4,860 9,241 10,456 Amortization of convertible senior notes and
lease financing obligations 7,395 6,781 14,685 13,455 Other, net
5,077 3,271 8,641 1,723 Changes in operating assets and
liabilities: Receivables (139,694 ) (135,282 ) (34,668 ) (174,579 )
Prepaid expenses and other current assets 40,251 11,136 (97,027 )
(66,887 ) Medical claims and benefits payable 44,120 104,641
291,730 254,395 Amounts due government agencies 202,776 76,607
297,741 119,872 Accounts payable and accrued liabilities (31,639 )
(1,327 ) 157,734 57,625 Deferred revenue (112,088 ) (100,331 )
(138,353 ) (76,271 ) Income taxes (440 ) 11,374 1,409
16,016 Net cash provided by operating activities 94,077
24,563 647,710 235,460 Investing
activities: Purchases of investments (554,387 ) (226,159 ) (992,978
) (368,304 ) Proceeds from sales and maturities of investments
285,441 179,278 541,050 326,648
Purchases of property, equipment, and
capitalized software
(40,886 ) (19,882 ) (65,860 ) (37,670 ) Increase in restricted
investments (9,590 ) (1,241 ) (14,202 ) (15,622 ) Net cash paid in
business combinations — — (8,006 ) — Other, net (9,637 ) (6,841 )
(16,853 ) (7,388 ) Net cash used in investing activities (329,059 )
(74,845 ) (556,849 ) (102,336 ) Financing activities:
Proceeds from common stock offering, net of issuance costs 373,151
— 373,151 — Contingent consideration liabilities settled — (12,230
) — (50,349 ) Proceeds from employee stock plans 7,298 6,287 8,387
7,617 Other, net (1,609 ) 207 2,420 1,064 Net
cash provided by (used in) financing activities 378,840
(5,736 ) 383,958 (41,668 ) Net increase (decrease) in cash
and cash equivalents 143,858 (56,018 ) 474,819 91,456 Cash and cash
equivalents at beginning of period 1,870,024 1,083,369
1,539,063 935,895 Cash and cash equivalents at
end of period $ 2,013,882 $ 1,027,351 $ 2,013,882
$ 1,027,351
MOLINA HEALTHCARE, INC.UNAUDITED
NON-GAAP FINANCIAL MEASURES
The Company uses two non-GAAP financial measures as supplemental
metrics in evaluating its financial performance, making financing
and business decisions, and forecasting and planning for future
periods. For these reasons, management believes such measures are
useful supplemental measures to investors in comparing the
Company’s performance to the performance of other public companies
in the health care industry. These non-GAAP financial measures
should be considered as supplements to, and not as substitutes for
or superior to, GAAP measures.
The first of these non-GAAP measures is earnings before
interest, taxes, depreciation and amortization (EBITDA). The
following table reconciles net income, which the Company believes
to be the most comparable GAAP measure, to EBITDA.
Three Months Ended Six Months
Ended June 30, June 30, 2015
2014 2015 2014 (Amounts in
thousands) Net income $ 38,943 $ 7,811 $ 67,096 $ 12,309
Adjustments: Depreciation, and amortization of intangible assets
and capitalized software 28,688 28,292 57,798 54,206 Interest
expense 14,946 13,993 29,822 27,815 Income tax expense 61,799
10,760 101,039 15,997 EBITDA $ 144,376
$ 60,856 $ 255,755 $ 110,327
The second of these non-GAAP measures is adjusted net income,
continuing operations (including adjusted net income per diluted
share). The following table reconciles net income from continuing
operations, which the Company believes to be the most comparable
GAAP measure, to adjusted net income, continuing operations.
Three Months Ended June 30,
Six Months Ended June 30, 2015 2014
2015 2014 (In thousands, except per diluted
share amounts) Net income, continuing operations $ 38,931
$ 0.72 $ 7,741 $ 0.16 $ 67,072
$ 1.29 $ 12,575 $ 0.26 Adjustments, net of
tax: Amortization of convertible senior notes and lease financing
obligations 4,659 0.09 4,272 0.09 9,252 0.18 8,477 0.18
Amortization of intangible assets 2,671 0.05 3,209
0.07 5,548 0.10 6,538 0.14
Adjusted net income, continuing operations (1) $ 46,261 $
0.86 $ 15,222 $ 0.32 $ 81,872 $ 1.57
$ 27,590 $ 0.58
(1) Beginning in the first quarter of 2015, the Company revised
its calculation of adjusted net income, continuing operations. The
Company no longer subtracts “depreciation, and amortization of
capitalized software” and “share-based compensation” from net
income, continuing operations to arrive at adjusted net income,
continuing operations. The Company has made this change to better
reflect the way in which it evaluates its financial performance,
makes financing and business decisions, and forecasts and plans for
future periods. All periods presented conform to this
presentation.
MOLINA HEALTHCARE, INC.
UNAUDITED HEALTH PLANS SEGMENT
MEMBERSHIP, CONTINUING OPERATIONS
June 30,
2015
March 31,
2015
December 31,
2014
June 30,
2014
Ending Membership by Health Plan: California 593,000 574,000
531,000 455,000 Florida 348,000 352,000 164,000 58,000 Illinois
101,000 102,000 100,000 6,000 Michigan 260,000 256,000 242,000
244,000 New Mexico 225,000 222,000 212,000 195,000 Ohio 332,000
350,000 347,000 302,000
Puerto Rico (1)
361,000 — — — South Carolina 114,000 111,000 118,000 119,000 Texas
266,000 268,000 245,000 247,000 Utah 92,000 90,000 83,000 83,000
Washington 553,000 533,000 497,000 461,000 Wisconsin 107,000
107,000 84,000 85,000 3,352,000 2,965,000
2,623,000 2,255,000
Ending Membership by
Program: Temporary Assistance for Needy Families (TANF), CHIP
(2) 2,180,000 1,825,000 1,809,000 1,642,000 Medicaid Expansion (3)
475,000 437,000 385,000 232,000 Aged, Blind or Disabled (ABD)
353,000 358,000 347,000 314,000 Marketplace (3) 261,000 266,000
15,000 18,000 Medicare Special Needs Plans 44,000 45,000 49,000
44,000 Medicare-Medicaid Plan (MMP) – Integrated (4) 39,000
34,000 18,000 5,000 3,352,000 2,965,000
2,623,000 2,255,000
(1) The Puerto Rico health plan began
serving members effective April 1, 2015.
(2) CHIP stands for Children’s Health
Insurance Program.
(3) Medicaid Expansion membership phased
in, and Marketplace became available for consumers
to access coverage, beginning January 1,
2014.
(4) MMP members who receive both Medicaid
and Medicare coverage from the Company. The Company began serving
members under this program in the second quarter of 2014.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA,
CONTINUING OPERATIONS
(In thousands, except percentages and
per-member per-month amounts)
Three Months Ended June 30, 2015 Member
Months (1)
Premium Revenue Medical Care Costs
MCR (2)
Medical
Margin
Total PMPM Total PMPM
California 1,767 $ 503,739 $ 285.14 $ 459,045 $ 259.85 91.1 % $
44,694 Florida 1,053 257,317 244.35 216,906 205.97 84.3 40,411
Illinois 301 101,769 337.55 98,260 325.91 96.6 3,509 Michigan 773
237,506 307.27 199,940 258.67 84.2 37,566 New Mexico 690 321,808
466.46 276,144 400.27 85.8 45,664 Ohio 996 508,468 510.30 432,186
433.75 85.0 76,282 Puerto Rico 1,082 193,984 179.33 184,240 170.32
95.0 9,744 South Carolina 337 93,089 276.36 66,332 196.92 71.3
26,757 Texas 806 512,408 635.74 468,629 581.42 91.5 43,779 Utah 277
79,964 288.60 71,727 258.88 89.7 8,237 Washington 1,643 409,758
249.39 370,437 225.46 90.4 39,321 Wisconsin 320 74,532 233.15
56,140 175.62 75.3 18,392 Other (3) — 10,030 — 29,548
— — (19,518 ) 10,045 $ 3,304,372 $ 328.96 $
2,929,534 $ 291.65 88.7 % $ 374,838
Three
Months Ended June 30, 2014 Member
Months (1)
Premium Revenue Medical Care Costs MCR
(2)
Medical
Margin
Total PMPM Total PMPM California 1,335
$ 398,071 $ 298.11 $ 324,923 $ 243.33 81.6 % $ 73,148 Florida 229
101,423 443.05 92,865 405.67 91.6 8,558 Illinois 17 19,263 1,136.20
20,472 1,207.48 106.3 (1,209 ) Michigan 702 185,337 264.18 163,392
232.89 88.2 21,945 New Mexico 617 267,994 434.57 240,151 389.42
89.6 27,843 Ohio 849 328,630 386.79 276,716 325.69 84.2 51,914
Puerto Rico — — — — — — — South Carolina 360 96,453 268.38 84,686
235.64 87.8 11,767 Texas 742 320,966 432.46 297,899 401.38 92.8
23,067 Utah 249 76,574 307.47 73,094 293.49 95.5 3,480 Washington
1,364 336,959 247.03 305,098 223.67 90.5 31,861 Wisconsin 256
36,925 144.42 33,143 129.63 89.8 3,782 Other (3) — (1,453 )
— 21,860 — — (23,313 ) 6,720 $ 2,167,142 $
322.52 $ 1,934,299 $ 287.87 89.3 % $ 232,843
(1) A member month is defined as the
aggregate of each month’s ending membership for the period
presented.
(2) The MCR represents medical costs as a
percentage of premium revenue.
(3) “Other” medical care costs include
primarily medically related administrative costs at the parent
company, and direct delivery costs.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA,
CONTINUING OPERATIONS
(In thousands, except percentages and
per-member per-month amounts)
Six Months Ended June 30, 2015 Member
Months (1)
Premium Revenue Medical Care Costs
MCR (2)
Medical
Margin
Total PMPM Total PMPM
California 3,440 $ 1,014,283 $ 294.85 $ 911,480 $ 264.97 89.9 % $
102,803 Florida 1,950 568,288 291.33 498,295 255.45 87.7 69,993
Illinois 606 205,914 339.72 187,697 309.66 91.2 18,217 Michigan
1,529 457,031 298.87 384,703 251.57 84.2 72,328 New Mexico 1,374
635,464 462.62 567,970 413.48 89.4 67,494 Ohio 2,051 1,023,555
498.96 845,260 412.05 82.6 178,295 Puerto Rico 1,082 193,984 179.33
184,240 170.32 95.0 9,744 South Carolina 680 184,415 271.35 140,601
206.88 76.2 43,814 Texas 1,581 894,193 565.45 820,107 518.60 91.7
74,086 Utah 543 157,106 289.42 145,871 268.72 92.8 11,235
Washington 3,206 786,108 245.22 722,811 225.47 91.9 63,297
Wisconsin 622 134,874 216.85 104,849 168.58 77.7 30,025 Other (3) —
19,809 — 51,434 — — (31,625 ) 18,664 $
6,275,024 $ 336.21 $ 5,565,318 $ 298.18 88.7 % $
709,706
Six Months Ended June 30, 2014
Member
Months (1)
Premium Revenue Medical Care Costs MCR
(2)
Medical
Margin
Total PMPM Total PMPM California 2,589
$ 675,713 $ 260.97 $ 562,267 $ 217.16 83.2 % $ 113,446 Florida 499
206,589 414.17 186,326 373.55 90.2 20,263 Illinois 31 34,434
1,109.99 34,966 1,127.12 101.5 (532 ) Michigan 1,350 358,833 265.81
298,712 221.27 83.2 60,121 New Mexico 1,166 493,062 423.00 436,560
374.53 88.5 56,502 Ohio 1,621 606,925 374.33 514,044 317.04 84.7
92,881 Puerto Rico — — — — — — — South Carolina 754 192,473 255.31
174,948 232.07 90.9 17,525 Texas 1,491 641,062 429.85 590,857
396.19 92.2 50,205 Utah 495 155,228 313.67 140,294 283.49 90.4
14,934 Washington 2,640 660,420 250.15 603,205 228.48 91.3 57,215
Wisconsin 530 75,453 142.48 61,952 116.99 82.1 13,501 Other (3) —
7,287 — 51,826 — — (44,539 ) 13,166 $
4,107,479 $ 311.98 $ 3,655,957 $ 277.69 89.0 % $
451,522
(1) A member month is defined as the
aggregate of each month’s ending membership for the period
presented.
(2) The MCR represents medical costs as a
percentage of premium revenue.
(3) “Other” medical care costs include
primarily medically related administrative costs at the parent
company, and direct delivery costs.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA,
CONTINUING OPERATIONS
(In thousands, except percentages and
per-member per-month amounts)
Three Months Ended June 30, 2015 (1)
Member
Months (2)
Premium Revenue Medical Care Costs
MCR (3)
Medical
Margin
Total PMPM Total PMPM
TANF and CHIP 6,556 $ 1,169,277 $ 178.38 $ 1,063,489 $ 162.24 91.0
% $ 105,788 Medicaid Expansion 1,387 582,443 419.67 474,198 341.67
81.4 108,245 ABD 1,069 1,053,098 984.99 947,093 885.84 89.9 106,005
Marketplace 789 161,214 204.22 89,368 113.21 55.4 71,846 Medicare
133 140,137 1,059.90 140,508 1,062.71 100.3 (371 ) MMP 111
198,203 1,784.30 214,878 1,934.40 108.4 (16,675 )
10,045 $ 3,304,372 $ 328.96 $ 2,929,534 $
291.65 88.7 % $ 374,838
Six Months Ended June 30,
2015 (1) Member
Months (2)
Premium Revenue Medical Care Costs MCR
(3)
Medical
Margin
Total PMPM Total PMPM TANF and CHIP
12,035 $ 2,141,316 $ 177.93 $ 1,960,315 $ 162.89 91.5 % $ 181,001
Medicaid Expansion 2,661 1,089,339 409.29 867,229 325.84 79.6
222,110 ABD 2,120 1,993,366 940.23 1,809,613 853.56 90.8 183,753
Marketplace 1,371 354,725 258.66 245,682 179.15 69.3 109,043
Medicare 264 273,472 1,036.95 269,005 1,020.01 98.4 4,467 MMP 213
422,806 1,986.04 413,474 1,942.20 97.8 9,332
18,664 $ 6,275,024 $ 336.21 $ 5,565,318
$ 298.18 88.7 % $ 709,706
(1) Three and six months ended June 30,
2014 data not presented due to lack of comparability.
(2) A member month is defined as the
aggregate of each month’s ending membership for the period
presented.
(3) The MCR represents medical costs as a
percentage of premium revenue.
MOLINA HEALTHCARE, INC. UNAUDITED SELECTED
HEALTH PLANS SEGMENT FINANCIAL DATA, CONTINUING
OPERATIONS (In thousands, except percentages and per-member
per-month amounts)
The following tables provide the details
of the Company’s medical care costs from continuing operations for
the periods indicated:
Three Months Ended June 30, 2015
2014 Amount PMPM % of
Total
Amount PMPM % of
Total
Fee for service $ 2,102,776 $ 209.34 71.8 % $ 1,378,037 $ 205.08
71.2 % Pharmacy 391,899 39.01 13.3 295,596 43.99 15.3 Capitation
248,357 24.72 8.5 176,817 26.31 9.1 Direct delivery 27,885 2.78 1.0
23,063 3.43 1.2 Other 158,617 15.80 5.4 60,786
9.06 3.2 $ 2,929,534 $ 291.65
100.0 % $ 1,934,299 $ 287.87 100.0 %
Six
Months Ended June 30, 2015 2014 Amount
PMPM % of
Total
Amount PMPM % of
Total
Fee for service $ 4,051,081 $ 217.05 72.8 % $ 2,559,098 $ 194.38
70.0 % Pharmacy 743,097 39.81 13.4 582,224 44.22 15.9 Capitation
464,682 24.90 8.3 346,256 26.30 9.5 Direct delivery 54,656 2.93 1.0
45,084 3.42 1.2 Other 251,802 13.49 4.5
123,295 9.37 3.4 $ 5,565,318 $ 298.18
100.0 % $ 3,655,957 $ 277.69 100.0 %
The following table provides the details
of the Company’s medical claims and benefits payable as of the
dates indicated:
June 30,
2015
December 31,
2014
Fee-for-service claims incurred but not paid (IBNP) $ 1,138,794 $
870,429 Pharmacy payable 80,902 71,412 Capitation payable 30,673
28,150 Other (1) 241,883 230,531 $ 1,492,252 $
1,200,522
(1) “Other” medical claims and
benefits payable include amounts payable to certain providers for
which the Company acts as an intermediary on behalf of various
state agencies without assuming financial risk. Such receipts and
payments do not impact the Company’s unaudited consolidated
statements of income. As of June 30, 2015 and December 31, 2014,
the Company had recorded non-risk provider payables of
approximately $134.2 million and $119.3 million, respectively.
MOLINA HEALTHCARE, INC.UNAUDITED
CHANGE IN MEDICAL CLAIMS AND BENEFITS PAYABLE(Dollars in
thousands, except per-member amounts)
The Company’s claims liability includes an allowance for adverse
claims deviation based on historical experience and other factors
including, but not limited to, variations in claims payment
patterns, changes in utilization and cost trends, known outbreaks
of disease, and large claims. The Company’s reserving methodology
is consistently applied across all periods presented. The amounts
displayed for “Components of medical care costs related to: Prior
period” represent the amount by which the Company’s original
estimate of claims and benefits payable at the beginning of the
period were more than the actual amount of the liability based on
information (principally the payment of claims) developed since
that liability was first reported. The following table presents the
components of the change in medical claims and benefits payable
from continuing and discontinued operations combined for the
periods indicated:
Six Months Ended
Year Ended
December 31,
2014
June 30, 2015 2014 Medical
claims and benefits payable, beginning balance $ 1,200,522 $
669,787 $ 669,787 Components of medical care costs related to:
Current period 5,703,391 3,693,730 8,122,885 Prior period (1)
(138,131 ) (37,131 ) (45,979 ) Total medical care costs 5,565,260
3,656,599 8,076,906 Change in non-risk
provider payables 14,826 (83,044 ) (31,973 ) Payments for
medical care costs related to: Current period 4,448,820 2,891,174
7,064,427 Prior period 839,536 427,986 449,771
Total paid 5,288,356 3,319,160 7,514,198
Medical claims and benefits payable, ending balance $ 1,492,252
$ 924,182 $ 1,200,522 Benefit from
prior period as a percentage of: Balance at beginning of period
11.5 % 5.5 % 6.9 % Premium revenue, trailing twelve months 1.2 %
0.5 % 0.5 % Medical care costs, trailing twelve months 1.4 % 0.6 %
0.6 % Fee-For-Service Claims Data: Days in claims payable,
fee for service 49 46 49 Number of members at end of year 3,352,000
2,255,000 2,623,000 Number of claims in inventory at end of year
463,200 180,600 307,700 Billed charges of claims in inventory at
end of year $ 904,800 $ 400,000 $ 718,500 Claims in inventory per
member at end of year 0.14 0.08 0.12 Billed charges of claims in
inventory per member at end of year $ 269.93 $ 177.38 $ 273.92
Number of claims received during the year 18,679,000 12,641,300
27,597,000 Billed charges of claims received during the year $
21,505,000 $ 13,609,000 $ 30,315,600
(1) The benefit from prior
period development of medical claims and benefits payable for the
six months ended June 30, 2015, included approximately $22
million relating to programs that contain medical cost floor or
corridor provisions. Accordingly, premium revenue for the six
months ended June 30, 2015, was reduced by the same amount.
MOLINA HEALTHCARE, INC.
HEALTH INSURER FEE DETAILS BY HEALTH
PLAN
(In thousands)
HIF Reimbursement Revenue, Gross (1) Six
Months Ended June 30, 2015
Year Ending
Dec. 31, 2015
Recognized
Necessary
for
Full Reimbursement
Necessary
for
Full Reimbursement
Q1 2015 Q2 2015 Total 2015
HIF: California $ — $ 17,258 $ 17,258 $ 17,258 $ 34,517 Florida
2,027 2,042 4,069 4,069 8,139 Illinois 965 973 1,938 1,938 3,875
Michigan — — — 13,776 27,551 New Mexico 7,539 7,597 15,136 15,136
30,273 Ohio 11,936 12,027 23,963 23,963 47,925 South Carolina 3,053
3,077 6,130 6,130 12,261 Texas 5,839 5,884 11,723 11,723 23,446
Utah — — — 2,968 5,936 Washington 10,951 10,963 21,914 21,914
43,828 Wisconsin 1,126 1,135 2,261 2,261
4,522 Subtotal, Medicaid 43,436 60,956 104,392
121,136 242,273 Marketplace 398 400 798 798 1,595 Medicare 5,702
3,652 9,354 9,354 18,702 49,536 65,008
114,544 $ 131,288 $ 262,570
2014 HIF: California —
11,616 11,616 $ 49,536 $ 76,624
$ 126,160
Recognized in: Health insurer fee
revenue $ 47,948 $ 73,890 $ 121,838 Premium tax revenue 1,588
2,734 4,322 $ 49,536 $ 76,624 $
126,160
(1) Amounts in the table
include the Company’s estimate of the full economic impact of the
excise tax including premium tax and the income tax effect.
View source
version on businesswire.com: http://www.businesswire.com/news/home/20150730006504/en/
Molina Healthcare, Inc.Investor Relations:Juan José Orellana,
562-435-3666, ext. 111143
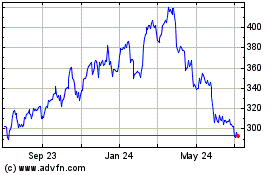
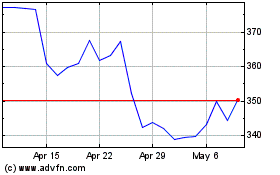
Molina Healthcare (NYSE:MOH)
Historical Stock Chart
From Aug 2024 to Sep 2024
Molina Healthcare (NYSE:MOH)
Historical Stock Chart
From Sep 2023 to Sep 2024