Aetna to Drop Some Affordable Care Act Markets
August 15 2016 - 10:40PM
Dow Jones News
Aetna Inc. will withdraw from 11 of the 15 states where it
currently offers plans through the Affordable Care Act exchanges,
becoming the latest of the major national health insurers to pull
back sharply from the law's signature marketplaces after steep
financial losses.
Aetna's move will sharpen concerns about competitive options in
the exchanges—and it puts at least one county, Pinal in Arizona, at
risk of having no insurers offering exchange plans in 2017, a
circumstance that would present a major challenge to the basic
mechanics of the ACA.
The law mandates that most people acquire health coverage, and
offers subsidies to lower-income consumers who don't qualify for
Medicaid. To obtain the subsidies, though, people are supposed to
purchase their plans through ACA exchanges.
Stephen Briggs, a spokesman for Arizona's state insurance
regulator, said the state currently has no insurers that have filed
to offer exchange plans in Pinal, a county in the Phoenix area.
"It's a concern for us," he said, but the regulator doesn't "have
any legal leverage to compel anyone to offer a plan." However, the
regulator is speaking to other insurers about offering exchange
plans in Pinal, he said, and "circumstances could change."
A spokesman for the federal Department of Health and Human
Services said, "we are working collaboratively with the Arizona
Department of Insurance and remain confident that all Arizona
residents will have access to coverage next year."
Blue Cross Blue Shield of Arizona said in June that it would
withdraw from Pinal County and Maricopa County, in the wake of
steep losses, but maintain its exchange presence in the remainder
of the state. The nonprofit had said in June that it stayed in
more-rural counties partly because it "couldn't overlook that
several counties would have no options or very limited access if we
didn't find a way to stay in the market." A spokeswoman had no
immediate comment late Monday.
Aetna will reduce the number of counties where it sells exchange
plans next year to 242 from 778, a dramatic turn that came a few
weeks after the insurer said it expected steep losses for the year
and would reconsider its participation in the market, which it had
previously called an important opportunity.
The insurer earlier this month also said it would cancel a
potential expansion into five new states. Aetna has been a major
player in ACA business, with about 1.1 million individual
enrollees, roughly 838,000 of whom purchased their coverage on the
exchanges.
In a statement, Aetna Chief Executive Mark T. Bertolini said the
pullback will "limit our financial exposure moving forward," and
added that Aetna "may expand our footprint in the future should
there be meaningful exchange-related policy improvements."
Aetna's move comes after UnitedHealth Group Inc. and Humana Inc.
already unveiled major reductions in their ACA-plan offerings, and
as more nonprofit cooperative insurers have said they will
fold.
"I see an erosion of freedom of choice," said Jim O'Connor, a
principal at consultants Milliman Inc., both among different
insurers but also among health-care providers, as more exchange
plans feature limited networks of hospitals and doctors.
In a statement, Kevin Counihan, a Department of Health and Human
Services official who oversees the federal marketplace, said
Aetna's decision "does not change the fundamental fact that the
Health Insurance Marketplace will continue to bring quality
coverage to millions of Americans next year and every year after
that."
The four states where Aetna will remain on the ACA exchanges are
Delaware, Iowa, Nebraska and Virginia. The insurer said it will
maintain a considerably broader footprint for selling individual
plans off the exchanges.
The list of states where Aetna will no longer offer ACA exchange
plans includes around nine where UnitedHealth too is pulling
out—among them are Arizona, North Carolina, Kentucky and South
Carolina.
Already, Aetna's previously announced decision to cancel
possible expansions meant that Oklahoma, where it had filed to
begin selling ACA plans, is likely to become the latest state with
just one marketplace insurer next year. Others are likely to
include Alabama, Alaska and Wyoming.
The withdrawals come as the biggest insurers continue to roll up
losses on their ACA business—all five major national companies now
expect to be in the red on that business this year. Aetna said it
expected a loss of more than $300 million for the year on its ACA
plans amid mounting medical costs among enrollees. The insurer lost
about $200 million in the second quarter on the plans.
A number of other insurers, many focused largely on Medicaid
plans, have said their ACA business is doing well, and they will
maintain or expand it.
Write to Anna Wilde Mathews at anna.mathews@wsj.com
(END) Dow Jones Newswires
August 15, 2016 22:25 ET (02:25 GMT)
Copyright (c) 2016 Dow Jones & Company, Inc.
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Mar 2024 to Apr 2024
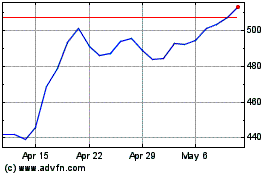
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Apr 2023 to Apr 2024
