UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
Form 8-K
CURRENT REPORT
Pursuant
to Section 13 or 15(d)
of the Securities Exchange Act of 1934
Date of Report (date of earliest event reported): April 14, 2015
DAVITA HEALTHCARE PARTNERS INC.
(Exact name of registrant as specified in its charter)
|
|
|
|
|
| Delaware |
|
1-14106 |
|
No. 51-0354549 |
| (State or other jurisdiction
of incorporation) |
|
(Commission
File Number) |
|
(IRS Employer
Identification No.) |
2000 16th Street
Denver, CO 80202
(Address
of principal executive offices including Zip Code)
(303) 405-2100
(Registrant’s telephone number, including area code)
Not applicable
(Former
name or former address, if changed since last report)
Check the appropriate box below
if the Form 8-K filing is intended to simultaneously satisfy the filing obligation of the registrant under any of the following provisions:
| ¨ |
Written communications pursuant to Rule 425 under the Securities Act (17 CFR 240.425) |
| ¨ |
Soliciting material pursuant to Rule 14a-12 under the Exchange Act (17 CFR 240.14a-12) |
| ¨ |
Pre-commencement communications pursuant to Rule 14d-2(b) under the Exchange Act (17 CFR 240.14d-2(b)) |
| ¨ |
Pre-commencement communications pursuant to Rule 13e-4(c) under the Exchange Act (17 CFR 240.13e-4(c)) |
Item 8.01. Other Events.
On April 14, 2015, the Board of Directors of DaVita HealthCare Partners Inc. (the “Company”) approved an additional share
repurchase program of approximately $725,944,000 (the “New Repurchase Program”). The amount of shares of common stock authorized to be repurchased under the New Repurchase Program is in addition to the amount remaining under the
Company’s existing stock repurchase program (the “Existing Repurchase Program”) announced on November 4, 2010. As of the date hereof, approximately $274,056,000 remains available under the Existing Repurchase Program. The
Existing Purchase Program and the New Repurchase Program do not have an expiration date and do not obligate the Company to purchase any shares. Repurchases under the New Repurchase Program and the Existing Repurchase Program may take place in the
open market or privately negotiated transactions, including without limitation, accelerated share repurchase transactions, derivative transactions, and under Rule 10b5-1 plans. There can be no assurance as to the precise number of
shares that will be repurchased under the New Repurchase Program, the aggregate dollar amount of the shares purchased, or the ultimate disposition of the shares purchased (re-issued, retained in treasury and/or retired). Depending on market
conditions, regulatory, legal and contractual requirements and other factors, repurchases may be made at any time or from time to time, without prior notice. The Company may suspend or discontinue the Existing Purchase Program and the New Repurchase
Program, or increase or decrease the amount of shares authorized to be repurchased thereunder, at any time.
The Company is also filing this Form 8-K for
the purpose of incorporating by reference the updated “Risk Factors” relating to the Company’s business, attached hereto as Exhibit 99.1 and incorporated by reference herein, into the Company’s Registration Statement on Form S-3
(and the related prospectus contained therein and any applicable prospectus supplement thereto) to be filed with the U.S. Securities and Exchange Commission immediately following the filing of this Form 8-K. References in such updated “Risk
Factors” to the “Company,” “we,” “us” or “our” are references to DaVita HealthCare Partners Inc. and its consolidated subsidiaries, except as the context otherwise requires.
This Current Report on Form 8-K and the documents incorporated by reference herein contain or may contain statements that are forward-looking statements
within the meaning of Section 27A of the Securities Act of 1933, as amended and Section 21E of the Securities Exchange Act of 1934, as amended. We intend these forward-looking statements to be covered by the safe harbor provisions for such
statements. All statements that do not concern historical facts are forward-looking statements and include, among other things, statements about our expectations, beliefs, intentions and/or strategies for the future. These forward-looking statements
include statements regarding anticipated refinancing transactions, our future operations, financial condition and prospects, expectations for treatment growth rates, revenue per treatment, expense growth, levels of the provision for uncollectible
accounts receivable, operating income, cash flow, operating cash flow, estimated tax rates, capital expenditures, the development of new dialysis centers and dialysis center acquisitions, government and commercial payment rates, revenue estimating
risk and the impact of our level of indebtedness on our financial performance, including earnings per share. These statements can sometimes be identified by the use of forward looking words such as “may,” “believe,”
“will,” “should,” “could,” “would,” “expect,” “project,” “estimate,” “anticipate,” “plan,” “continue,” “seek,” “forecast,” or
“intend” or other similar words or expressions of the negative thereof. These statements involve substantial known and unknown risks and uncertainties that could cause our actual results to differ materially from those described in the
forward-looking statements, including, but not limited to the risk factors set forth in Item 1A of the Company’s Annual Report on Form 10-K for the year ended December 31, 2014 and the additional risk factors attached hereto.
Item 9.01. Financial Statements and Exhibits.
(d)
Exhibits.
|
|
|
| Exhibit
No. |
|
Description |
|
|
| 99.1 |
|
Risk Factors Relating to the Company’s Business, updated as of April 14, 2015. |
SIGNATURES
Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by
the undersigned hereunto duly authorized.
|
|
|
|
|
|
|
|
|
|
|
DAVITA HEALTHCARE PARTNERS INC. |
|
|
|
|
| Date: April 14, 2015 |
|
|
|
By: |
|
/s/ Kim M. Rivera |
|
|
|
|
|
|
Kim M. Rivera |
|
|
|
|
|
|
Chief Legal Officer |
EXHIBIT INDEX
|
|
|
| Exhibit
No. |
|
Description |
|
|
| 99.1 |
|
Risk Factors Relating to the Company’s Business, updated as of April 14, 2015. |
Exhibit 99.1
Risks Relating to Our Business
Risk factors related
to our U.S. dialysis and related lab services, ancillary services and strategic initiatives:
If the average rates that commercial payors pay us
decline significantly, it would have a material adverse effect on our revenues, earnings and cash flows.
Approximately 33% of our
dialysis and related lab services revenues for the year ended December 31, 2014, were generated from patients who have commercial payors as their primary payor. The majority of these patients have insurance policies that pay us on terms and at
rates that are generally significantly higher than Medicare rates. The payments we receive from commercial payors generate nearly all of our profit and all of our nonacute dialysis profits come from commercial payors. We continue to experience
downward pressure on some of our commercial payment rates as a result of general conditions in the market, recent and future consolidations among commercial payors, increased focus on dialysis services and other factors. There is no guarantee that
commercial payment rates will not be materially lower in the future.
We are continuously in the process of negotiating our existing or
potentially new agreements with commercial payors who tend to be aggressive in their negotiations with us. Sometimes many significant agreements are up for renewal or being renegotiated at the same time. In the event that our continual negotiations
result in overall commercial rate reductions in excess of overall commercial rate increases, the cumulative effect could have a material adverse effect on our financial results. Consolidations have significantly increased the negotiating leverage of
commercial payors. Our negotiations with payors are also influenced by competitive pressures, and we may experience decreased contracted rates with commercial payors or experience decreases in patient volume as our negotiations with commercial
payors continue. In addition to downward pressure on contracted commercial payor rates, payors have been attempting to impose restrictions and limitations on non-contracted or out-of-network providers, and in some circumstances designate our centers
as out-of-network providers. Rates for out-of-network providers are on average higher than rates for in-network providers. We believe commercial payors have or will begin to restructure their benefits to create disincentives for patients to select
or remain with out-of-network providers and to decrease payment rates for out-of-network providers. Decreases in out-of-network rates and restrictions on out-of-network access, our turning away new patients in instances where we are unable to come
to agreement on rates, or decreases in contracted rates could result in a significant decrease in our overall revenues derived from commercial payors. If the average rates that commercial payors pay us decline significantly, or if we see a decline
in commercial patients, it would have a material adverse effect on our revenues, earnings and cash flows. For additional details regarding specific risks we face regarding regulatory changes that could result in fewer patients covered under
commercial plans or an increase of patients covered under more restrictive commercial plans with lower reimbursement rates, see the discussion of individual and small group health plans in the risk factor below under the heading “Health care
reform could substantially reduce our revenues, earnings and cash flows.”
S-1
If the number of patients with higher-paying commercial insurance declines, then our revenues, earnings and
cash flows would be substantially reduced.
Our revenue levels are sensitive to the percentage of our patients with higher-paying
commercial insurance coverage. A patient’s insurance coverage may change for a number of reasons, including changes in the patient’s or a family member’s employment status. Currently, for a patient covered by an employer group health
plan, Medicare generally becomes the primary payor after 33 months, or earlier, if the patient’s employer group health plan coverage terminates. When Medicare becomes the primary payor, the payment rate we receive for that patient decreases
from the employer group health plan rate to the lower Medicare payment rate. We have seen an increase in the number of patients who have government-based programs as their primary payors which we believe is largely a result of improved mortality and
recent economic conditions which have a negative impact on the percentage of patients covered under commercial insurance plans. To the extent there are sustained or increased job losses in the U.S., independent of whether general economic conditions
might be improving, we could experience a continued decrease in the number of patients covered under commercial plans. We could also experience a further decrease if changes to the healthcare regulatory system result in fewer patients covered under
commercial plans or an increase of patients covered under more restrictive commercial plans with lower reimbursement rates. In addition, our continuous process of negotiations with commercial payors under existing or potentially new agreements could
result in a decrease in the number of patients under commercial plans to the extent that we cannot reach agreement with commercial payors on rates and other terms, resulting in termination or non-renewals of existing agreements or our inability to
enter into new ones. If there is a significant reduction in the number of patients under higher-paying commercial plans relative to government-based programs that pay at lower rates, it would have a material adverse effect on our revenues, earnings
and cash flows.
Changes in the structure of and payment rates under the Medicare End Stage Renal Disease (ESRD) program could substantially reduce
our revenues, earnings and cash flows.
Approximately 47% of our dialysis and related lab services revenues for the year ended
December 31, 2014 was generated from patients who have Medicare as their primary payor. For patients with Medicare coverage, all ESRD payments for dialysis treatments are made under a single bundled payment rate which provides a fixed payment
rate to encompass all goods and services provided during the dialysis treatment, including pharmaceuticals that were historically separately reimbursed to the dialysis providers, such as Epogen (EPO), vitamin D analogs and iron supplements,
irrespective of the level of pharmaceuticals administered or additional services performed. Most lab services that used to be paid directly to laboratories are also included in the bundled payment. The bundled payment rate is also adjusted for
certain patient characteristics, a geographic usage index and certain other factors.
The current bundled payment system presents certain
operating, clinical and financial risks, which include:
| |
• |
|
Risk that our rates are reduced by Center for Medicare and Medicaid Services (CMS). Uncertainty about future payment rates remains a material risk to our business. CMS issued the 2014 final rule for the ESRD prospective
payment system (PPS), which phases in the payment reductions mandated by the American Taxpayer Relief Act of 2012 (ATRA) as modified by the “Protecting Access to Medicare Act” which will reduce our market basket inflation adjustment
by—1.25% in 2016 and 2017, and 1% in 2018. CMS also recently issued the 2015 final rule for the ESRD PPS, which will increase payments to dialysis facilities modestly by 0.3% to 0.5%, although rural facilities will receive a decrease of 0.5%.
|
| |
• |
|
Risk that increases in our operating costs will outpace the Medicare rate increases we receive. We expect to continue experiencing increases in operating costs that are subject to inflation, such as labor and supply
costs, regardless of whether there is a compensating inflation-based increase in Medicare payment rates or in payments under the bundled payment rate system. |
| |
• |
|
Risk of federal budget sequestration cuts. As a result of the Budget Control Act of 2011 (BCA) and subsequent activity in Congress, a $1.2 trillion
sequester (across-the-board spending cuts) in discretionary programs took effect on March 1, 2013. In particular, a 2% reduction to Medicare |
S-2
| |
payments took effect on April 1, 2013, which was subsequently extended through 2014 and 2015. The across-the-board spending cuts pursuant to the sequester have affected and will continue to
adversely affect our revenues, earnings and cash flows. |
| |
• |
|
Risk that if our clinical systems fail to accurately capture the data we report to CMS in connection with claims for which at least part of the government’s payments to us is based on clinical performance or
patient outcomes or co-morbidities, we might be over-reimbursed by the government which could subject us to certain liability. For example, the False Claims Act (FCA) requires the return of overpayments in a timely fashion or claims associated with
those overpayments are subject to FCA penalties. |
For additional details regarding the risks we face for failing to adhere
to our Medicare and Medicaid regulatory compliance obligations, see the risk factor below under the heading “If we fail to adhere to all of the complex government regulations that apply to our business, we could suffer severe consequences that
would substantially reduce our revenues, earnings, cash flows and stock price.”
Healthcare reform could substantially reduce our revenues,
earnings and cash flows.
We cannot predict how employers, private payors or persons buying insurance might react to the changes
brought on by broad U.S. healthcare reform legislation or what form many of these regulations will take before implementation.
The
healthcare reform legislation introduced healthcare insurance exchanges which provide a marketplace for eligible individuals and small employers to purchase healthcare insurance. Although we cannot predict the short or long term effects of these
measures, we believe the healthcare insurance exchanges could result in a reduction in ESRD patients covered by traditional commercial insurance policies and an increase in the number of patients covered through the exchanges under more restrictive
commercial plans with lower reimbursement rates or higher deductibles and co-payments that patients may not be able to pay. To the extent that the implementation of such exchanges results in a reduction in patients covered by commercial insurance or
a reduction in reimbursement rates for our services from commercial and/or government payors, our revenues, earnings and cash flows could be adversely affected.
In addition, the healthcare reform legislation introduced severe penalties for the knowing and improper retention of overpayments collected
from government payors and reduced the timeline to file Medicare claims. As a result, we made significant initial investments in new resources to accelerate the time it takes us to identify and process overpayments and we deployed significant
resources to reduce our timeline and improve our claims processing methods to ensure that our Medicare claims are filed in a timely fashion. We may be required to make additional investments in the future. Failure to timely identify and return
overpayments may result in significant penalties, which may have a negative impact on our revenues, earnings and cash flows. Failure to file a claim within the one year window could result in payment denials, adversely affecting our revenues,
earnings and cash flows.
The healthcare reform legislation also added several new tax provisions that, among other things, impose various
fees and excise taxes, and limit compensation deductions for health insurance providers and their affiliates. These rules could negatively impact our cash flow and tax liabilities.
CMS Center for Medicare & Medicaid Innovation (Innovation Center) is currently working with various healthcare providers to develop,
refine and implement accountable care organizations (ACOs) and other innovative models of care for Medicare and Medicaid beneficiaries. We are currently uncertain of the extent to which the long-term operation and evolution of these care models,
including ACOs, Bundled Payments for Care Improvement Initiative, Comprehensive ESRD Care Model (which includes the development of ESCOs), the Comprehensive Primary Care Initiative, the Duals Demonstration, and other models, will impact the
healthcare market over time. Our U.S. dialysis business may choose to participate in one or several of these models either as a partner with other providers or independently. We are currently seeking to participate in the Comprehensive ESRD Care
Model with Innovation Center. Even if we do not participate in this or other programs, some of our patients may be
S-3
assigned to a program, in which case the quality and cost of care that we furnish will be included in an ACO’s or other programs’ calculations. As new models of care emerge and evolve,
we may be at risk of losing our Medicare patient base, which would have a materially adverse effect on our revenues, earnings and cash flow. Other initiatives in the government or private sector may arise, including the development of models similar
to ACOs, IPAs and integrated delivery systems or evolutions of those concepts which could adversely impact our business.
CMS instituted
new screening procedures which we expect will delay the Medicare contractor approval process, potentially causing a delay in reimbursement. We anticipate the new screening and enrollment requirements will require additional personnel and financial
resources and will potentially delay the enrollment and revalidation of our centers which in turn will delay payment. These delays may negatively impact our revenues, earnings and cash flows.
Other reform measures allow CMS to place a moratorium on new enrollment of providers and to suspend payment to providers upon a credible
allegation of fraud from any source. These types of reform measures, as well as other measures, could adversely impact our revenues, earnings and cash flows depending upon the scope and breadth of the implementing regulations.
There is also a considerable amount of uncertainty as to the prospective implementation of the federal healthcare reform legislation and what
similar measures might be enacted at the state level. The enacted reforms as well as future legislative changes could have a material adverse effect on our results of operations, including lowering our reimbursement rates and increasing our
expenses.
Changes in state Medicaid or other non-Medicare government-based programs or payment rates could reduce our revenues, earnings and cash
flows.
Approximately 20% of our dialysis and related lab services revenues for the year ended December 31, 2014 was generated
from patients who have state Medicaid or other non-Medicare government-based programs, such as coverage through the Department of Veterans Affairs (VA), as their primary coverage. As state governments and other governmental organizations face
increasing budgetary pressure, we may in turn face reductions in payment rates, delays in the receipt of payments, limitations on enrollee eligibility or other changes to the applicable programs. For example, certain state Medicaid programs and the
VA have recently considered, proposed or implemented payment rate reductions.
The VA adopted Medicare’s bundled PPS pricing
methodology for any veterans receiving treatment from non-VA providers under a national contracting initiative. Since we are a non-VA provider, these reimbursements are tied to a percentage of Medicare reimbursement, and we have exposure to any
dialysis reimbursement changes made by CMS. Approximately 2% of our dialysis and related lab services revenues for the year ended December 31, 2014 was generated by the VA.
In 2013, we entered into a five-year Nationwide Dialysis Services contract with the VA which is subject to one-year renewal periods,
consistent with all provider agreements with the VA under this contract. During the length of the contract, the VA has elected not to make adjustments to reimbursement percentages that are tied to a percentage of Medicare reimbursement rates. These
agreements provide the VA with the right to terminate the agreements without cause on short notice. Should the VA not renew or cancel these agreements for any reason, we may cease accepting patients under this program and may be forced to close
centers, which could adversely affect our revenues, earnings and cash flows.
State Medicaid programs are increasingly adopting
Medicare-like bundled payment systems, but sometimes these payment systems are poorly defined and are implemented without any claims processing infrastructure, or patient or facility adjusters. If these payment systems are implemented without any
adjusters and claims processing changes, Medicaid payments will be substantially reduced and the costs to submit such claims may increase, which will have a negative impact on our revenues, earnings and cash flows. In addition, some state
S-4
Medicaid program eligibility requirements mandate that citizen enrollees in such programs provide documented proof of citizenship. If our patients cannot meet these proof of citizenship
documentation requirements, they may be denied coverage under these programs, resulting in decreased patient volumes and revenue. These Medicaid payment and enrollment changes, along with similar changes to other non-Medicare government programs
could reduce the rates paid by these programs for dialysis and related services, delay the receipt of payment for services provided, and further limit eligibility for coverage which could adversely affect our revenues, earnings and cash flows.
Changes in clinical practices, payment rates or regulations impacting EPO and other pharmaceuticals could adversely affect our operating results, reduce
our revenues, earnings and cash flows and negatively impact our ability to care for patients.
Medicare bundles EPO into the
prospective payment system such that dosing variations do not change the amount paid to a dialysis facility. Although some Medicaid programs and other payors suggest movement towards a bundled payment system inclusive of EPO, some non-Medicare
payors continue to pay for EPO separately from the treatment rate. The administration of EPO and other pharmaceuticals that are separately billable accounted for approximately 3% of our dialysis and related lab services revenues for the year ended
December 31, 2014, with EPO alone accounting for approximately 2% of our dialysis and related lab services revenues during that period. Changes in physician clinical practices that result in further decreased utilization of prescribed
pharmaceuticals or changes in payment rates for those pharmaceuticals could reduce our revenues, earnings and cash flows.
Evaluations on
the utilization and reimbursement for erythropoiesis stimulating agents (ESAs), which have occurred in the past and may occur in the future, and related actions by the U.S. Congress and federal agencies, could result in further restrictions on the
utilization and reimbursement for ESAs. Additionally, commercial payors have increasingly examined their administration policies for EPO and, in some cases, have modified those policies. Changes in labeling of EPO and other pharmaceuticals in a
manner that alters physician practice patterns or accepted clinical practices, changes in private and governmental payment criteria, including the introduction of EPO administration policies or the conversion to alternate types of administration of
EPO or other pharmaceuticals that result in further decreases in utilization of EPO for patients covered by commercial payors could have a material adverse effect on our revenues, earnings and cash flows. Further increased utilization of EPO for
patients for whom the cost of EPO is included in a bundled reimbursement rate, or further decreases in reimbursement for EPO and other pharmaceuticals that are not included in a bundled reimbursement rate, could also have a material adverse effect
on our revenues, earnings and cash flows.
Additionally, as a result of the current high level of scrutiny and controversy, we may be
subject to increased inquiries or audits from a variety of governmental bodies or claims by third parties. Although we believe our anemia management practices and other pharmaceutical administration practices have been compliant with existing laws
and regulations, increased inquiries or audits from governmental bodies or claims by third parties would require management’s attention, and could result in significant legal expense. Any negative findings could result in substantial financial
penalties or repayment obligations, the imposition of certain obligations on and changes to our practices and procedures as well as the attendant financial burden on us to comply with the obligations, or exclusion from future participation in the
Medicare and Medicaid programs, and could have a material adverse effect on our revenues, earnings and cash flows.
Changes in EPO pricing could
materially reduce our earnings and cash flows and affect our ability to care for our patients.
Future increases in the cost of EPO
without corresponding increases in payment rates for EPO from commercial payors and without corresponding increases in the Medicare bundled rate could have a material adverse effect on our earnings and cash flows and ultimately reduce our income. In
November 2011, we entered into a seven year Sourcing and Supply Agreement with Amgen USA Inc., pursuant to which we committed to purchase EPO in amounts necessary to meet no less than 90% of our requirements for ESAs. As long as we meet
S-5
certain conditions, the agreement limits Amgen’s ability to unilaterally increase the price for EPO during the term of the agreement. Our agreement with Amgen provides for discounted pricing
and rebates for EPO. However, some of the rebates are subject to various conditions including, but not limited to, future pricing levels of EPO by Amgen and data submission by us. In addition, the rebates are subject to certain limitations. We
cannot predict whether, over the seven year term of the agreement, we will continue to receive the rebates for EPO that we have received in the past, or whether we will continue to achieve the same levels of rebates within that structure as we have
historically achieved. Factors that could impact our ability to qualify for rebates provided for in our agreement with Amgen in the future include, but are not limited to, our ability to track certain data elements. We cannot predict whether we will
be able to meet the applicable qualification requirements for receiving rebates. Failure to meet certain targets and earn the specified rebates could have a material adverse effect on our earnings and cash flows.
If we fail to comply with our Corporate Integrity Agreement, we could be subject to substantial penalties and exclusion from participation in federal
healthcare programs that may adversely impact our revenues, earnings and cash flows.
In October 2014, we entered into a Settlement
Agreement with the United States and relator David Barbetta to resolve the pending 2010 and 2011 U.S. Attorney Physician Relationship Investigations and paid $406 million in settlement amounts, civil forfeiture, and interest to the United States and
certain States. In connection with the resolution of these matters, and in exchange for the OIG’s agreement not to exclude us from participating in the federal healthcare programs, we have entered into the five-year Corporate Integrity
Agreement (CIA) with the OIG. The CIA (i) requires that we maintain certain elements of our compliance programs, (ii) imposes certain expanded compliance-related requirements during the term of the CIA, (iii) requires ongoing
monitoring and reporting by an independent monitor, reporting, certification, records retention and training obligations, the formal allocation of certain oversight responsibility to the Board’s Compliance Committee, the creation of a
Management Compliance Committee and the retention of an independent compliance advisor to the Board, and (iv) contains certain business restrictions related to a subset of our joint venture arrangements, including our agreeing to:
(1) unwind 11 joint venture transactions that were created through partial divestitures to or partial acquisitions from nephrologists and that cover 26 of our 2,119 clinics that existed at the time we entered into the Settlement Agreement;
(2) not enter into certain types of partial divestiture joint venture transactions with nephrologists during the term of the CIA; and (3) non-enforcement of certain patient-related non-solicitation restrictions; (4) and certain other
restrictions. The costs associated with compliance with the CIA could be substantial and may be greater than we currently anticipate. In addition, in the event of a breach of the CIA, we could become liable for payment of certain stipulated
penalties and could be excluded from participation in federal healthcare programs. The costs associated with compliance with the CIA, or any liability or consequences associated with its breach, could have an adverse effect on our revenues, earnings
and cash flows.
If we fail to adhere to all of the complex government regulations that apply to our business, we could suffer severe consequences
that would substantially reduce our revenues, earnings, cash flows and stock price.
Our dialysis operations are subject to
extensive federal, state and local government regulations, including Medicare and Medicaid payment rules and regulations, federal and state anti-kickback laws, the physician self-referral law (Stark Law) and analogous state self-referral prohibition
statutes, Federal Acquisition Regulations, the FCA and federal and state laws regarding the collection, use and disclosure of patient health information and the storage, handling and administration of pharmaceuticals. The Medicare and Medicaid
reimbursement rules related to claims submission, enrollment and licensing requirements, cost reporting, and payment processes impose complex and extensive requirements upon dialysis providers as well. A violation or departure from any of these
legal requirements may result in government audits, lower reimbursements, significant fines and penalties, the potential loss of certification, recoupment efforts or voluntary repayments.
We endeavor to comply with all legal requirements, however, there is no guarantee that we will be able to adhere to all of the complex
government regulations that apply to our business. We further endeavor to structure all of our relationships with physicians to comply with state and federal anti-kickback and physician self-referral
S-6
laws. We utilize considerable resources to monitor the laws and implement necessary changes. However, the laws and regulations in these areas are complex and often subject to varying
interpretations. For example, if an enforcement agency were to challenge the level of compensation that we pay our medical directors or the number of medical directors whom we engage, we could be required to change our practices, face criminal or
civil penalties, pay substantial fines or otherwise experience a material adverse effect as a result of a challenge to these arrangements. In addition, amendments to the FCA impose severe penalties for the knowing and improper retention of
overpayments collected from government payors. These amendments could subject our procedures for identifying and processing overpayments to greater scrutiny. We have made significant investments in new resources to decrease the time it takes to
identify and process overpayments and we may be required to make additional investments in the future. An acceleration in our ability to identify and process overpayments could result in us refunding overpayments to government and other payors more
rapidly than we have in the past which could have a material adverse effect on our operating cash flows. Additionally, amendments to the federal anti-kickback statute in the health reform law make anti-kickback violations subject to FCA prosecution,
including qui tam or whistleblower suits.
If any of our operations are found to violate these or other government regulations, we could
suffer severe consequences that would have a material adverse effect on our revenues, earnings, cash flows and stock price, including:
| |
• |
|
Suspension or termination of our participation in government payment programs; |
| |
• |
|
Refunds of amounts received in violation of law or applicable payment program requirements; |
| |
• |
|
Loss of required government certifications or exclusion from government payment programs; |
| |
• |
|
Loss of licenses required to operate healthcare facilities or administer pharmaceuticals in some of the states in which we operate; |
| |
• |
|
Reductions in payment rates or coverage for dialysis and ancillary services and related pharmaceuticals; |
| |
• |
|
Fines, damages or monetary penalties for anti-kickback law violations, Stark Law violations, FCA violations, civil or criminal liability based on violations of law, or other failures to meet regulatory requirements;
|
| |
• |
|
Enforcement actions by governmental agencies and/or state claims for monetary damages by patients who believe their protected health information has been used, disclosed or not properly safeguarded in violation of
federal or state patient privacy laws, including Health Insurance Portability and Accountability Act (HIPAA) of 1996; |
| |
• |
|
Mandated changes to our practices or procedures that significantly increase operating expenses; |
| |
• |
|
Imposition of and compliance with corporate integrity agreements that could subject us to ongoing audits and reporting requirements as well as increased scrutiny of our billing and business practices which could lead to
potential fines; |
| |
• |
|
Termination of relationships with medical directors; and |
| |
• |
|
Harm to our reputation which could impact our business relationships, affect our ability to obtain financing and decrease access to new business opportunities. |
Delays in state Medicare and Medicaid certification of our dialysis centers could adversely affect our revenues, earnings and cash flows.
Before we can begin billing for patients treated in our outpatient dialysis centers who are enrolled in government-based programs, we are
required to obtain state and federal certification for participation in the Medicare and Medicaid programs. As state agencies responsible for surveying dialysis centers on behalf of the
S-7
state and Medicare program face increasing budgetary pressure, certain states are having difficulty keeping up with certifying dialysis centers in the normal course resulting in significant
delays in certification. If state governments continue to have difficulty keeping up with certifying new centers in the normal course and we continue to experience significant delays in our ability to treat and bill for services provided to patients
covered under government programs, it could cause us to incur write-offs of investments or accelerate the recognition of lease obligations in the event we have to close centers or our centers’ operating performance deteriorates, and it could
have an adverse effect on our revenues, earnings and cash flows.
If our joint ventures were found to violate the law, we could suffer severe
consequences that would have a material adverse effect on our revenues, earnings and cash flows.
As of December 31, 2014, we
owned a controlling interest in numerous dialysis-related joint ventures, which represented approximately 22% of our U.S. dialysis and related lab services revenues for the year ended December 31, 2014. In addition, we also owned minority
equity investments in several other dialysis related joint ventures. We may continue to increase the number of our joint ventures. Many of our joint ventures with physicians or physician groups also have certain physician owners providing medical
director services to centers we own and operate. Because our relationships with physicians are governed by the federal and state anti-kickback statutes, we have sought to structure our joint venture arrangements to satisfy as many federal safe
harbor requirements as we believe are commercially reasonable. However, although our joint venture arrangements do not satisfy all of the elements of any safe harbor under the federal anti-kickback statute, they are not automatically prohibited
under the federal anti-kickback statute but are susceptible to government scrutiny. In October 2014, we entered into a Settlement Agreement with the United States and relator David Barbetta to resolve the then pending 2010 and 2011 U.S. Attorney
Physician Relationship Investigations regarding certain of our joint ventures and paid $406 million in settlement amounts, civil forfeiture, and interest to the United States and certain States. For further details, please see “If we fail to
comply with our CIA, we could be subject to substantial penalties and exclusion from participation in federal healthcare programs that may adversely impact our revenues, earnings and cash flows”.
There are significant estimating risks associated with the amount of dialysis revenues and related refund liabilities that we recognize and if we are
unable to accurately estimate our revenues and related refund liabilities, it could impact the timing and the amount of our revenues recognition or have a significant impact on our operating results.
There are significant estimating risks associated with the amount of dialysis and related lab services revenues and related refund liabilities
that we recognize in a reporting period. The billing and collection process is complex due to ongoing insurance coverage changes, geographic coverage differences, differing interpretations of contract coverage, and other payor issues. Determining
applicable primary and secondary coverage for approximately 173,000 U.S. patients at any point in time, together with the changes in patient coverage that occur each month, requires complex, resource-intensive processes. Errors in determining the
correct coordination of benefits may result in refunds to payors. Revenues associated with Medicare and Medicaid programs are also subject to estimating risk related to the amounts not paid by the primary government payor that will ultimately be
collectible from other government programs paying secondary coverage, the patient’s commercial health plan secondary coverage or the patient. Collections, refunds and payor retractions typically continue to occur for up to three years and
longer after services are provided. We generally expect our range of U.S. dialysis and related lab services revenues estimating risk to be within 1% of net revenues for the segment, which represents approximately 5% of dialysis and related lab
services adjusted operating income. If our estimates of dialysis and related lab services revenues and related refund liabilities are materially inaccurate, it could impact the timing and the amount of our revenues recognition and have a significant
impact on our operating results.
S-8
Our ancillary services and strategic initiatives, including our international dialysis operations, that we
invest in now or in the future may generate losses and may ultimately be unsuccessful. In the event that one or more of these activities is unsuccessful, we may have to write off our investment and incur other exit costs.
Our ancillary services and strategic initiatives currently include pharmacy services, disease management services, vascular access services,
ESRD clinical research programs, physician services, direct primary care and our international dialysis operations. We expect to add additional service offerings and pursue additional strategic initiatives in the future as circumstances warrant,
which could include healthcare services not related to dialysis. Many of these initiatives require or would require investments of both management and financial resources and can generate significant losses for a substantial period of time and may
not become profitable. There can be no assurance that any such strategic initiative will ultimately be successful. Any significant change in market conditions, or business performance, or in the political, legislative or regulatory environment, may
impact the economic viability of any of these strategic initiatives. If any of our ancillary services or strategic initiatives, including our international dialysis operations, do not perform as planned, we may incur a material write-off or an
impairment of our investment, including goodwill, in one or more of these activities or we could incur significant termination costs if we were to exit a certain line of business.
If a significant number of physicians were to cease referring patients to our dialysis centers, whether due to regulatory or other reasons, it would
have a material adverse effect on our revenues, earnings and cash flows.
We believe that physicians prefer to have their patients
treated at dialysis centers where they or other members of their practice supervise the overall care provided as medical director of the center. As a result, the primary referral source for most of our centers is often the physician or physician
group providing medical director services to the center.
Our medical director contracts are for fixed periods, generally ten years, and
at any given time a large number of them could be up for renewal at the same time. Medical directors have no obligation to extend their agreements with us and if we are unable to enforce noncompetition provisions contained in terminated medical
director agreements, our former medical directors may choose to provide medical director services for competing providers or establish their own dialysis centers in competition with ours. Neither our current nor former medical directors have an
obligation to refer their patients to our centers.
Opportunities presented by our competitors or different affiliation models in the
changing healthcare environment, such as an increase in the number of physicians becoming employed by hospitals or a perceived decrease in the quality of service levels at our centers may negatively impact a medical director’s decision to enter
into or extend his or her agreement with us, refer patients to our centers or otherwise negatively impact treatment volumes.
In addition,
we may take actions to restructure existing relationships or take positions in negotiating extensions of relationships to assure compliance with the anti-kickback statute, Stark Law and other similar laws. If the terms of any existing agreement are
found to violate applicable laws, we may not be successful in restructuring the relationship which could lead to the early termination of the agreement, or cause the physician to stop referring patients to our dialysis centers. These actions in an
effort to comply with applicable laws and regulations could negatively impact the decision of physicians to extend their medical director agreements with us or to refer their patients to us. If a significant number of physicians were to cease
referring patients to our dialysis centers, our revenues, earnings and cash flows would be substantially reduced.
Deterioration in economic
conditions as well as further disruptions in the financial markets could have a material adverse effect on our revenues, earnings and cash flows and otherwise adversely affect our financial condition.
Deterioration in economic conditions could adversely affect our business and our profitability. Among other things, the potential decline in
federal and state revenues that may result from such conditions may create
S-9
additional pressures to contain or reduce reimbursements for our services from Medicare, Medicaid and other government sponsored programs. Increasing job losses or slow improvement in the
unemployment rate in the U.S. as a result of adverse economic conditions has and may continue to result in a smaller percentage of our patients being covered by an employer group health plan and a larger percentage being covered by lower paying
Medicare and Medicaid programs. Employers may also select more restrictive commercial plans with lower reimbursement rates. To the extent that payors are negatively impacted by a decline in the economy, we may experience further pressure on
commercial rates, a further slowdown in collections and a reduction in the amounts we expect to collect. In addition, uncertainty in the financial markets could adversely affect the variable interest rates payable under our credit facilities or
could make it more difficult to obtain or renew such facilities or to obtain other forms of financing in the future, if at all. Any or all of these factors, as well as other consequences of a deterioration in economic conditions which cannot
currently be anticipated, could have a material adverse effect on our revenues, earnings and cash flows and otherwise adversely affect our financial condition.
If there are shortages of skilled clinical personnel or if we experience a higher than normal turnover rate, we may experience disruptions in our
business operations and increases in operating expenses.
We are experiencing increased labor costs and difficulties in hiring
nurses due to a nationwide shortage of skilled clinical personnel. We compete for nurses with hospitals and other healthcare providers. This nursing shortage may limit our ability to expand our operations. In addition, changes in certification
requirements or increases in the required staffing levels for skilled clinical personnel can impact our ability to maintain sufficient staff levels to the extent our teammates are not able to meet new requirements or we experience a higher than
normal turnover rate due to increased competition for qualified clinical personnel. If we are unable to hire skilled clinical personnel when needed, or if we experience a higher than normal turnover rate for our skilled clinical personnel, our
operations and treatment growth will be negatively impacted, which would result in reduced revenues, earnings and cash flows.
Our business is labor
intensive and could be adversely affected if we are unable to maintain satisfactory relations with our employees or if union organizing activities result in significant increases in our operating costs or decreases in productivity.
Our business is labor intensive, and our results are subject to variations in labor-related costs, productivity and the number of pending or
potential claims against us related to labor and employment practices. If political efforts at the national and local level result in actions or proposals that increase the likelihood of union organizing activities at our facilities or if union
organizing activities increase for other reasons, or if labor and employment claims, including the filing of class action suits, trend upwards, our operating costs could increase and our employee relations, productivity, earnings and cash flows
could be adversely affected.
Complications associated with our migration to a new billing and collections system could have a material adverse
effect on our revenues, cash flows and operating results.
We are launching a new billing system that is critical to our billing
operations. If the launch is unsuccessful or if there are defects in the new billing system, we may experience difficulties in our ability to successfully bill and collect for services rendered, including a delay in collections, a reduction in the
amounts collected, increased risk of retractions from and refunds to commercial and government payors, an increase in our provision for uncollectible accounts receivable and noncompliance with reimbursement regulations. To mitigate this risk, we are
launching the new system in phases; however, the failure to successfully implement the new billing and collection system could have a material adverse effect on our revenues, cash flows and operating results.
Our ability to effectively provide the services we offer could be negatively impacted if certain of our suppliers are unable to meet our needs or if we
are unable to effectively access new technology, which could substantially reduce our revenues, earnings and cash flows.
We have
significant suppliers that are either the sole or primary source of products critical to the services we provide, including Amgen, Baxter Healthcare Corporation, NxStage Medical, Inc. and others or to which we
S-10
have committed obligations to make purchases including Gambro and FMC. If any of these suppliers are unable to meet our needs for the products they supply, including in the event of a product
recall or shortage, and we are not able to find adequate alternative sources, or if some of the drugs that we purchase are not reimbursed or not adequately reimbursed by commercial payors or through the bundled payment rate by Medicare, our
revenues, earnings and cash flows could be substantially reduced. In addition, the technology related to the products critical to the services we provide is subject to new developments and may result in superior products. If we are not able to
access superior products on a cost-effective basis or if suppliers are not able to fulfill our requirements for such products, we could face patient attrition which could substantially reduce our revenues, earnings and cash flows.
Risk factors related to HealthCare Partners (HCP):
HCP is subject to many of the same risks to which our dialysis business is subject.
As a participant in the healthcare industry, HCP is subject to many of the same risks to which our dialysis business is subject to as described
in the risk factors set forth above, any of which could materially and adversely affect HCP’s revenues, earnings or cash flows. Among these risks are the following:
| |
• |
|
The healthcare business is heavily regulated and changes in laws, regulations, or government programs could have a material impact on HCP; |
| |
• |
|
Failure to comply with complex governmental regulations could have severe consequences to HCP, including, without limitation, exclusion from governmental payor programs like Medicare and Medicaid; |
| |
• |
|
HCP could become the subject of governmental investigations, claims, and litigation; |
| |
• |
|
HCP may be unable to continue to explore potential acquisition candidates, make acquisitions or successfully integrate such acquisitions into its business, and such acquisitions may include liabilities of which HCP was
not aware; and |
| |
• |
|
As a result of the broad scope of HCP’s medical practice, HCP is exposed to medical malpractice claims, as well as claims for damages and other expenses, that may not be covered by insurance or for which adequate
limits of insurance coverage may not be available. |
Under most of HCP’s agreements with health plans, HCP assumes some or all of
the risk that the cost of providing services will exceed its compensation.
Over 90% of HCP’s revenue is derived from fixed
Per Member Per Month (PMPM) fees paid by health plans under capitation agreements with HCP or its associated physician groups. While there are variations specific to each arrangement, HCP, through DaVita HealthCare Partners Plan, Inc., a subsidiary
of HealthCare Partners Holdings, LLC and a restricted Knox-Keene licensed entity (DaVita HealthCare Partners Plan), and, in certain instances, HCP’s associated physician groups generally contract with health plans to receive a PMPM fee for
professional services and assume the financial responsibility for professional services only. In some cases, the health plans separately enter into capitation contracts with third parties (typically hospitals) who receive directly a PMPM fee and
assume contractual financial responsibility for hospital services. In other cases, the health plan does not pay any portion of the PMPM fee to the hospital, but rather administers claims for hospital expenses itself. In both scenarios, HCP enters
into managed care-related administrative services agreements or similar arrangements with those third parties (typically hospitals) under which HCP agrees to be responsible for utilization review, quality assurance, and other managed care-related
administrative functions and claim payments. As compensation for such administrative services, HCP is entitled to receive a percentage of the amount by which the institutional capitation revenue received from health plans exceeds institutional
expenses; any such risk-share amount to which HCP is entitled is recorded as medical revenues and HCP is also responsible for a percentage of any short-fall in the event that institutional expenses exceed institutional revenues. To the extent that
members require more care than is anticipated, aggregate fixed PMPM amounts, or capitation
S-11
payments, may be insufficient to cover the costs associated with treatment. If medical expenses exceed estimates, except in very limited circumstances, HCP will not be able to increase the PMPM
fee received under these risk agreements during their then-current terms and could, directly or indirectly through its contracts with its associated physician groups, suffer losses with respect to such agreements.
Changes in HCP’s or its associated physician groups’ anticipated ratio of medical expense to revenue can significantly impact
HCP’s financial results. Accordingly, the failure to adequately predict and control medical expenses and to make reasonable estimates and maintain adequate accruals for incurred but not reported claims, may have a material adverse effect on
HCP’s financial condition, results of operations or cash flows.
Historically, HCP’s and its associated physician groups’
medical expenses as a percentage of revenue have fluctuated. Factors that may cause medical expenses to exceed estimates include:
| |
• |
|
the health status of members; |
| |
• |
|
higher than expected utilization of new or existing healthcare services or technologies; |
| |
• |
|
an increase in the cost of healthcare services and supplies, including pharmaceuticals, whether as a result of inflation or otherwise; |
| |
• |
|
changes to mandated benefits or other changes in healthcare laws, regulations, and practices; |
| |
• |
|
periodic renegotiation of provider contracts with specialist physicians, hospitals, and ancillary providers; |
| |
• |
|
periodic renegotiation of contracts with HCP’s affiliated primary care physicians and specialists; |
| |
• |
|
changes in the demographics of the participating members and medical trends; |
| |
• |
|
contractual or claims disputes with providers, hospitals, or other service providers within a health plan’s network; |
| |
• |
|
the occurrence of catastrophes, major epidemics, or acts of terrorism; and |
| |
• |
|
the reduction of health plan premiums. |
Risk-sharing arrangements that HCP and its associated physician
groups have with health plans and hospitals could result in their costs exceeding the corresponding revenues, which could reduce or eliminate any shared risk profitability.
Most of the agreements between health plans and HCP and its associated physician groups contain risk-sharing arrangements under which the
physician groups can earn additional compensation from the health plans by coordinating the provision of quality, cost-effective healthcare to members. However, such arrangements may require the physician group to assume a portion of any loss
sustained from these arrangements, thereby reducing HCP’s net income. Under these risk-sharing arrangements, HCP and its associated physician groups are responsible for a portion of the cost of hospital services or other services that are not
capitated. The terms of the particular risk-sharing arrangement allocate responsibility to the respective parties when the cost of services exceeds the related revenue, which results in a deficit, or permit the parties to share in any surplus
amounts when actual costs are less than the related revenue. The amount of non-capitated medical and hospital costs in any period could be affected by factors beyond the control of HCP, such as changes in treatment protocols, new technologies,
longer lengths of stay by the patient, and inflation. Certain of HCP’s agreements with health plans stipulate that risk-sharing pool deficit amounts are carried forward to offset any future years’ surplus amounts HCP would otherwise be
entitled to receive. HCP accrues for any such risk-sharing deficits. To the extent that such non-capitated medical and hospital costs are higher than anticipated, revenue may not be sufficient to cover the risk-sharing deficits the health plans and
HCP are responsible for, which could reduce HCP’s revenues and profitability.
S-12
Renegotiation, renewal, or termination of capitation agreements with health plans could have a significant
impact on HCP’s future profitability.
Under most of HCP’s and its associated physician groups’ capitation
agreements with health plans, the health plan is generally permitted to modify the benefit and risk obligations and compensation rights from time to time during the terms of the agreements. If a health plan exercises its right to amend its benefit
and risk obligations and compensation rights, HCP and its associated physician groups are generally allowed a period of time to object to such amendment. If HCP or its associated physician group so objects, under some of the risk agreements, the
relevant health plan may terminate the applicable agreement upon 90 to 180 days written notice. If HCP or its associated physician groups enter into capitation contracts or other risk sharing arrangements with unfavorable economic terms, or a
capitation contract is amended to include unfavorable terms, HCP could, directly or indirectly through its contracts with its associated physician groups, suffer losses with respect to such contract. Since HCP does not negotiate with CMS or any
health plan regarding the benefits to be provided under their Medicare Advantage plans, HCP often has just a few months to familiarize itself with each new annual package of benefits it is expected to offer. Depending on the health plan at issue and
the amount of revenue associated with the health plan’s risk agreement, the renegotiated terms or termination may have a material adverse effect on our HCP division and DaVita HealthCare Partners Inc.’s (DaVita’s) future revenues and
profitability.
Laws regulating the corporate practice of medicine could restrict the manner in which HCP is permitted to conduct its business and
the failure to comply with such laws could subject HCP to penalties or require a restructuring of HCP.
Some states have laws that
prohibit business entities, such as HCP, from practicing medicine, employing physicians to practice medicine, exercising control over medical decisions by physicians (also known collectively as the corporate practice of medicine) or engaging in
certain arrangements, such as fee-splitting, with physicians. In some states these prohibitions are expressly stated in a statute or regulation, while in other states the prohibition is a matter of judicial or regulatory interpretation. Of the
states in which HCP currently operates, California and Nevada prohibit the corporate practice of medicine.
In California and Nevada, HCP
operates by maintaining long-term contracts with its associated physician groups which are each owned and operated by physicians and which employ or contract with additional physicians to provide physician services. Under these arrangements, HCP
provides management services and, receives a management fee for providing non-medical management services; however, HCP does not represent that it offers medical services, and does not exercise influence or control over the practice of medicine by
the physicians or the associated physician groups.
In addition to the above management arrangements, HCP has certain contractual rights
relating to the orderly transfer of equity interests in certain of its associated California and Nevada physician groups through succession agreements and other arrangements with their physician equity holders. However, such equity interests cannot
be transferred to or held by HCP or by any non-professional organization. Accordingly, neither HCP nor HCP’s subsidiaries directly own any equity interests in any physician groups in California and Nevada. In the event that any of these
associated physician groups fails to comply with the management arrangement or any management arrangement is terminated and/or HCP is unable to enforce its contractual rights over the orderly transfer of equity interests in its associated physician
groups, such events could have a material adverse effect on HCP’s business, financial condition or results of operations.
It is
possible that a state regulatory agency or a court could determine that HCP’s agreements with physician equity holders of certain managed California and Nevada associated physician groups as described above, either independently or coupled with
the management services agreements with such associated physician groups, are in violation of the corporate practice of medicine doctrine. As a result, these arrangements could be deemed invalid, potentially resulting in a loss of revenues and an
adverse effect on results of operations derived from such associated physician groups. Such a determination could force a restructuring of HCP’s management arrangements with associated physician groups in California and/or Nevada, which might
include revisions of the
S-13
management services agreements, including a modification of the management fee and/or establishing an alternative structure, which would permit HCP to contract with a physician network without
violating the corporate practice of medicine prohibition. There can be no assurance that such a restructuring would be feasible, or that it could be accomplished within a reasonable time frame without a material adverse effect on HCP’s
operations and financial results. In December 2013, DaVita HealthCare Partners Plan obtained a restricted Knox-Keene license in California pursuant to the California Knox-Keene Health Care Service Plan Act of 1975 (the Knox-Keene Act), which permits
DaVita HealthCare Partners Plan to contract with health plans in California to accept global risk without violating the corporate practice of medicine prohibition. However, HCP’s Nevada associated physician groups and HCP, as well as those
physician equity holders of associated physician groups who are subject to succession agreements with HCP, could be subject to criminal or civil penalties or an injunction for practicing medicine without a license or aiding and abetting the
unlicensed practice of medicine.
If HCP’s agreements or arrangements with any physician equity holder(s) of associated physicians, physician
groups, or IPAs are deemed invalid under state law, including laws against the corporate practice of medicine, or federal law, or are terminated as a result of changes in state law, or if there is a change in accounting standards by the Financial
Accounting Standards Board (FASB) or the interpretation thereof affecting consolidation of entities, it could impact HCP’s consolidation of total revenues derived from such associated physician groups.
HCP’s financial statements are consolidated in accordance with applicable accounting standards and include the accounts of its
majority-owned subsidiaries and certain non-owned HCP-associated and managed physician groups. Such consolidation for accounting and/or tax purposes does not, is not intended to, and should not be deemed to, imply or provide to HCP any control over
the medical or clinical affairs of such physician groups. In the event of a change in accounting standards promulgated by FASB or in interpretation of its standards, or if there were an adverse determination by a regulatory agency or a court, or a
change in state or federal law relating to the ability to maintain present agreements or arrangements with such physician groups, HCP may not be permitted to continue to consolidate the total revenues of such organizations. A change in accounting
for consolidation with respect to HCP’s present agreement or arrangements would diminish HCP’s reported revenues but would not be expected to materially adversely affect its reported results of operations, while regulatory or legal rulings
or changes in law interfering with HCP’s ability to maintain its present agreements or arrangements could materially diminish both revenues and results of operations.
If DaVita HealthCare Partners Plan is not able to satisfy financial solvency or other regulatory requirements, DaVita HealthCare Partners Plan could
become subject to sanctions and its license to do business in California could be limited, suspended or terminated.
The Knox-Keene
Act requires healthcare service plans operating in California to comply with financial solvency and other requirements overseen by the California Department of Managed Health Care (DMHC). Under the Knox-Keene Act, DaVita HealthCare Partners Plan is
required to, among other things:
| |
• |
|
Maintain, at all times, a minimum tangible net equity; |
| |
• |
|
Submit periodic financial solvency reports to the DMHC containing various data regarding performance and financial solvency; |
| |
• |
|
Comply with extensive regulatory requirements; and |
| |
• |
|
Submit to periodic regulatory audits and reviews concerning DaVita HealthCare Partner Plan, Inc.’s operations and compliance with the Knox-Keene Act. |
In the event that DaVita HealthCare Partners Plan. is not in compliance with the provisions of the Knox-Keene Act, it could be subject to
sanctions, or limitations on, or suspension of its license to do business in California.
S-14
If HCP’s associated physician group is not able to satisfy the California Department of Managed Health
Care’s (DHMC’s) financial solvency requirements, HCP’s associated physician group could become subject to sanctions and HCP’s ability to do business in California could be limited or terminated.
The California DMHC has instituted financial solvency regulations to monitor the financial solvency of capitated physician groups. Under these
regulations, HCP’s associated physician group is required to, among other things:
| |
• |
|
Maintain, at all times, a minimum cash-to-claims ratio (where cash-to-claims ratio means the organization’s cash, marketable securities, and certain qualified receivables, divided by the organization’s total
unpaid claims liability). The regulation currently requires a cash-to-claims ratio of 0.75. |
| |
• |
|
Submit periodic reports to the California DMHC containing various data and attestations regarding performance and financial solvency, including incurred but not reported calculations and documentation, and attestations
as to whether or not the organization was in compliance with the Knox-Keene Act requirements related to claims payment timeliness had maintained positive tangible net equity (i.e., at least $1.00), and had maintained positive working capital (i.e.,
at least $1.00). |
In the event that HCP’s associated physician group is not in compliance with any of the above
criteria, HCP’s associated physician group could be subject to sanctions, or limitations on, or removal of, its ability to do business in California.
Reductions in Medicare Advantage health plan reimbursement rates stemming from recent healthcare reforms and any future related regulations may
negatively impact HCP’s business, revenue and profitability.
A significant portion of HCP’s revenue is directly or
indirectly derived from the monthly premium payments paid by CMS to health plans for medical services provided to Medicare Advantage enrollees. As a result, HCP’s results of operations are, in part, dependent on government funding levels for
Medicare Advantage programs. Any changes that limit or reduce Medicare Advantage reimbursement levels, including those recently approved and effective in 2014, such as reductions in or limitations of reimbursement amounts or rates under programs,
reductions in funding of programs, expansion of benefits without adequate funding, elimination of coverage for certain benefits, or elimination of coverage for certain individuals or treatments under programs, could have a material adverse effect on
HCP’s revenues, earnings and cash flows. On April 7, 2014 CMS issued final guidance for 2015 Medicare Advantage rates, which incorporated a re-blending of the risk adjustment models that CMS utilizes to determine risk acuity scores of
Medicare Advantage patients. In 2014, CMS blended the risk scores calculated using the 2013 CMS-HCC model and the 2014 CMS-HCC model by weighting the scores from the 2013 model by 25% and the scores from the 2014 model by 75%. In 2015, CMS will
blend the scores by 67% and 33%, respectively. Although we estimate that the final cumulative impact of the 2015 rate structure represents an increase of up to approximately 0.5% of HCP’s average Medicare Advantage revenues as compared to 2014,
there is no guarantee that CMS’s risk acuity adjustment models and the resulting Medicare Advantage rates will, in the future, increase HCP’s Medicare Advantage revenues.
On April 6, 2015, CMS issued its final rule establishing the 2016 Medicare Advantage benchmark payment rates as well as announcing the
model it will use to blend risk acuity scores. In 2016, CMS will blend the risk scores calculated using the 2013 CMS-HCC model and the 2014 CMS-HCC model by weighting the scores from the 2013 model by 0% and the scores from the 2014 model by 100%.
Based upon our preliminary analysis of the final rule, we estimate that the reduction in 2016 rates, including adjustments for the new ACA blended benchmark county rates and qualifying bonuses, will lead to a reduction in Medicare Advantage rates to
HCP of approximately 2%, or a net impact of approximately $50 million to our 2016 operating income. This compares to an industry average rate increase of approximately 1.25% as indicated by CMS in its final rule regarding the 2016 rates. The
final impact of 2016 Medicare Advantage rates can vary from this estimate and will be impacted by the relative growth of HCP’s Medicare Advantage patient volumes across markets as well as by the benefit plan designs submitted. It is possible
that we underestimated the impact of the 2016 Medicare Advantage rates on our business, and it has a material adverse effect on our financial position, results of operation or cash flows.
S-15
This more significant decline in Medicare Advantage rates for us compared to the industry average
is driven by a larger-than-average decline associated with CMS’s modification to the risk adjustment model calculation. The proposed move to the 2014 model negatively affects us and other providers like us who have differentially invested in
wellness and prevention programs for patients with chronic conditions, because the 2014 model tends to over-predict costs for very low-cost beneficiaries and under-predict costs for very high-cost beneficiaries.
In addition, we may need to take a goodwill impairment charge against earnings in the second quarter of 2015 relating to the impact of this
decrease in rates on the carrying value of net assets of our HCP reporting units. An impairment occurs when the carrying value of a reporting unit’s goodwill is in excess of its implied fair value. Although the amount of such non-cash charge,
if any, has not yet been determined, it could be significant. In estimating the fair value of our HCP reporting units, we will update our forecasts for each HCP reporting unit to reflect the expected future cash flows that we believe market
participants would use in determining the fair values of our HCP reporting units if they were to acquire these reporting units. We will also use certain estimates and key assumptions in determining our estimate of these fair values, including
discount and long-term growth rates, market data and future reimbursement rates. Our estimates of the fair value of our HCP reporting units could differ from the actual fair values a market participant would pay for these reporting units.
HCP’s Medicare Advantage revenues may continue to be volatile in the future, which could have a material impact on HCP’s ongoing
financial performance.
The Health Reform Acts contain a number of provisions that negatively impact Medicare Advantage plans, which may
each have an adverse effect on HCP’s revenues, earnings, and cash flows. These provisions include the following:
| |
• |
|
Medicare Advantage benchmarks for 2011 were frozen at 2010 levels. Beginning in 2012, Medicare Advantage benchmark rates are being phased down from prior levels to levels that are between 95% and 115% of the Medicare
FFS costs, depending on a plan’s geographic area. If our costs escalate faster than can be absorbed by the level of revenues implied by these benchmark rates, then it could have a significant negative impact on HCP’s earnings and cash
flows. |
| |
• |
|
Rebates received by Medicare Advantage plans that underbid based on payment benchmarks will be reduced, with larger reductions for plans failing to receive certain quality ratings. |
| |
• |
|
The Secretary of HHS has been granted the explicit authority to deny Medicare Advantage plan bids that propose significant increases in cost sharing or decreases in benefits. If the bids submitted by plans contracted
with HCP are denied, this would have a significant negative impact on HCP’s revenues, earnings and cash flows. |
| |
• |
|
Medicare Advantage plans with medical loss ratios below 85% are required to pay a rebate to the Secretary of the Department of Health and Human Services (HHS). The rebate amount is the total revenue under the contract
year multiplied by the difference between 85% and the plan’s actual medical loss ratio. The Secretary of HHS will halt enrollment in any plan failing to meet this ratio for three consecutive years, and terminate any plan failing to meet the
ratio for five consecutive years. If an HCP-contracting Medicare Advantage plan experiences a limitation on enrollment or is otherwise terminated from the Medicare Advantage program, HCP may suffer materially adverse consequences to its business or
financial condition. |
| |
• |
|
Prescription drug plans are now required to cover all drugs on a list developed by the Secretary of HHS, which could increase the cost of providing care to Medicare Advantage enrollees, and thereby reduce HCP’s
revenues and earnings. The Medicare part D premium subsidy for high-income beneficiaries has been reduced by 25%, which could lower the number of Medicare Advantage enrollees, which would have a negative impact on HCP’s revenues, earnings
and cash flows. |
| |
• |
|
CMS increased coding intensity adjustments for Medicare Advantage plans beginning in 2014 and continuing through 2018, which reduces CMS payments to Medicare Advantage plans, which in turn will likely reduce the amounts
payable to HCP and its associated physicians, physician groups, and IPAs under its capitation agreements. |
S-16
The President’s proposed 2015 budget proposed nearly $400 billion in cuts to Medicare,
Medicaid and other programs run by HHS over the next decade. Although the majority of the cuts are not targeted at Medicare Advantage plans, the broad cuts could signal further downward pressure on reimbursement to Medicare providers and Medicare
Advantage plans, which would have a negative impact on HCP’s revenues, earnings and cash flows. The final 2015 budget did not contain significant changes to Medicare funding, but cuts in future budgets could impact HCP’s revenues.
There is uncertainty regarding both Medicare Advantage payment rates and beneficiary enrollment, which, if reduced as a result of the
implementation of the Health Reform Acts, would reduce HCP’s overall revenues and net income. For example, although the Congressional Budget Office (CBO) predicted in 2012 that Medicare Advantage participation would drop precipitously by
2020, in 2013 the CBO reversed its prediction and instead predicted that enrollment in Medicare Advantage could increase by up to 50% in the next decade. Further fluctuation in Medicare Advantage payment rates were evidenced by CMS’s
announcement in its final 2015 “Call Letter” that Medicare Advantage rates would rise an average of 0.4% in 2015, instead of falling 1.9% as it had proposed in February 2014. On April 6, 2015, CMS announced its Medicare Advantage
rates for 2016. See above for further details. Uncertainty over Medicare Advantage enrollment and payment rates present a continuing risk to HCP’s business.
HCP’s operations are dependent on competing health plans and, at times, a health plan’s and HCP’s economic interests may diverge.
For the year ended December 31, 2014, 64% of HCP’s consolidated capitated medical revenues were earned through contracts
with three health plans.
HCP expects that, going forward, substantially all of its revenue will continue to be derived from its contracts
with health plans. Each health plan may immediately terminate any of HCP’s contracts and/or any individual credentialed physician upon the occurrence of certain events. They may also amend the material terms of the contracts under certain
circumstances. Failure to maintain the contracts on favorable terms, for any reason, would materially and adversely affect HCP’s results of operations and financial condition. A material decline in the number of members could also have a
material adverse effect on HCP’s results of operations.
Notwithstanding each health plan’s and HCP’s current shared
interest in providing service to HCP’s members who are enrolled in the subject health plans, the health plans may have different and, at times, opposing economic interests from those of HCP. The health plans provide a wide range of health
insurance services across a wide range of geographic regions, utilizing a vast network of providers. As a result, they and HCP may have different views regarding the proper pricing of services and/or the proper pricing of the various service
providers in their provider networks, the cost of which HCP bears to the extent that the services of such service providers are utilized. These health plans may also have different views than HCP regarding the efforts and expenditures that they,
HCP, and/or other service providers should make to achieve and/or maintain various quality ratings. In addition, several health plans have acquired or announced their intent to acquire provider organizations. If health plans with which HCP contracts
acquire a significant number of provider organizations, they may not continue to contract with HCP or contract on less favorable terms or seek to prevent HCP from acquiring or entering into arrangements with certain providers. Similarly, as a result
of changes in laws, regulations, consumer preferences, or other factors, the health plans may find it in their best interest to provide health insurance services pursuant to another payment or reimbursement structure. In the event HCP’s
interests diverge from the interests of the health plans, HCP may have limited recourse or alternative options in light of its dependence on these health plans. There can be no assurances that HCP will continue to find it mutually beneficial to work
with these health plans. As a result of various restrictive provisions that appear in some of the managed care agreements with health plans, HCP may at times have limitations on its ability to cancel an agreement with a particular health plan and
immediately thereafter contract with a competing health plan with respect to the same service area.
S-17
HCP and its associated physicians, physician groups and independent practice associations (IPAs) and other
physicians may be required to continue providing services following termination or renegotiation of certain agreements with health plans.
There are circumstances under federal and state law pursuant to which HCP and its associated physician groups IPAs, and other physicians could
be obligated to continue to provide medical services to HCP members in their care following a termination of their applicable risk agreement with health plans and termination of the receipt of payments thereunder. In certain cases, this obligation
could require the physician group or IPA to provide care to such member following the bankruptcy or insolvency of a health plan. Accordingly, the obligations to provide medical services to HCP members (and the associated costs) may not terminate at
the time the applicable agreement with the health plan terminates, and HCP may not be able to recover its cost of providing those services from the health plan, which could have a material adverse effect on HCP’s financial condition, results of
operations, and/or cash flows.
HCP operates primarily in Arizona, California, Florida, Nevada and New Mexico, and may not be able to successfully
establish a presence in new geographic regions.
HCP derives substantially all of its revenue from operations in Arizona,
California, Florida, Nevada and New Mexico (hereinafter referred to as the Existing Geographic Regions). As a result, HCP’s exposure to many of the risks described herein is not mitigated by a greater diversification of geographic focus.
Furthermore, due to the concentration of HCP’s operations in the Existing Geographic Regions, it may be adversely affected by economic conditions, natural disasters (such as earthquakes or hurricanes), or acts of war or terrorism that
disproportionately affect the Existing Geographic Regions as compared to other states and geographic markets.
To expand the operations of
its network outside of the Existing Geographic Regions, HCP must devote resources to identifying and exploring such perceived opportunities. Thereafter, HCP must, among other things, recruit and retain qualified personnel, develop new offices,
establish potentially new relationships with one or more health plans, and establish new relationships with physicians and other healthcare providers. The ability to establish such new relationships may be significantly inhibited by competition for
such relationships and personnel in the healthcare marketplace in the targeted new geographic regions. Additionally, HCP may face the risk that a substantial portion of the patients served in a new geographic area may be enrolled in a Medicare FFS
program and will not desire to transition to a Medicare Advantage program, such as those offered through the health plans that HCP serves, or they may enroll with other health plans with whom HCP does not contract to receive services, which could
reduce substantially HCP’s perceived opportunity in such geographic area. In addition, if HCP were to seek to expand outside of the Existing Geographic Regions, HCP would be required to comply with laws and regulations of states that may differ
from the ones in which it currently operates, and could face competitors with greater knowledge of such local markets. HCP anticipates that any geographic expansion may require it to make a substantial investment of management time, capital, and/or
other resources. There can be no assurance that HCP will be able to establish profitable operations or relationships in any new geographic markets.
Reductions in the quality ratings of the health plans HCP serves could have an adverse effect on its results of operations, financial condition, and/or
cash flow.
As a result of the Health Reform Acts, HCP anticipates that the level of reimbursement each health plan receives from
CMS will be dependent, in part, upon the quality rating of the Medicare plan that such health plan serves. Such ratings are expected to impact the percentage of any cost savings rebate and any bonuses earned by such health plan. Since a significant
portion of HCP’s revenue is expected to be calculated as a percentage of CMS reimbursements received by these health plans with respect to HCP members, reductions in the quality ratings of a health plan that HCP serves could have an adverse
effect on its results of operations, financial condition, and/or cash flows. In addition, CMS has announced its intention to terminate any plan that has a rating of less than three stars for three consecutive years. Medicare Advantage plans with
five stars are permitted to conduct enrollment throughout the year and enrollees in plans with 4.5 or fewer stars are permitted to change
S-18
plans during the year. Given each health plan’s control of its plans and the many other providers that serve such plans, HCP believes that it will have limited ability to influence the
overall quality rating of any such plan. Accordingly, since low quality ratings can potentially lead to the termination of a plan that HCP serves, HCP may not be able to prevent the potential termination of a contracting plan or a shift of patients
to other plans based upon quality issues which could, in turn, have an adverse effect on HCP’s results of operations, financial condition, and/or cash flows.
HCP’s records and submissions to a health plan may contain inaccurate or unsupportable information regarding risk adjustment scores of members,
which could cause HCP to overstate or understate its revenue and subject it to various penalties.
HCP, on behalf of itself and its
associated physicians, physician groups and IPAs, submits to health plans claims and encounter data that support the risk adjustment factor, or RAF, scores attributable to members. These RAF scores determine, in part, the revenue to which the health
plans and, in turn, HCP is entitled for the provision of medical care to such members. The data submitted to CMS by each health plan is based, in part, on medical charts and diagnosis codes prepared and submitted by HCP. Each health plan generally
relies on HCP to appropriately document and support such RAF data in HCP’s medical records. Each health plan also relies on HCP to appropriately code claims for medical services provided to members. HCP may periodically review medical records
and may find inaccurate or unsupportable coding or otherwise inaccurate records. Erroneous claims and erroneous encounter records and submissions could result in inaccurate PMPM fee revenue and risk adjustment payments, which may be subject to
correction or retroactive adjustment in later periods. This corrected or adjusted information may be reflected in financial statements for periods subsequent to the period in which the revenue was recorded. HCP might also need to refund a portion of
the revenue that it received, which refund, depending on its magnitude, could damage its relationship with the applicable health plan and could have a material adverse effect on HCP’s results of operations, financial condition or cash
flows. We have identified a potentially improper historical coding practice at HCP, which was discontinued following our acquisition of HCP. We have notified CMS and we intend to cooperate with government authorities to address this issue.
Additionally, CMS audits Medicare Advantage plans for documentation to support RAF-related payments for members chosen at random. The Medicare
Advantage plans ask providers to submit the underlying documentation for members that they serve. It is possible that claims associated with members with higher RAF scores could be subject to more scrutiny in a CMS audit. HCP has experienced
increases in RAF scores attributable to its members, and thus there is a possibility that a Medicare Advantage plan may seek repayment from HCP as a result of CMS payment adjustments to the Medicare Advantage plan. The plans also may hold HCP liable
for any penalties owed to CMS for inaccurate or unsupportable RAF scores provided by HCP. In addition, HCP could be liable for penalties to the government.
CMS has indicated that payment adjustments will not be limited to RAF scores for the specific Medicare Advantage enrollees for which errors
are found but may also be extrapolated to the entire Medicare Advantage plan subject to a particular CMS contract. CMS has described its audit process as plan-year specific and stated that it will not extrapolate audit results for plan years prior
to 2011. Because CMS has not stated otherwise, there is a risk that payment adjustments made as a result of one plan year’s audit would be extrapolated to prior plan years after 2011.
There can be no assurance that a health plan will not be randomly selected or targeted for review by CMS or that the outcome of such a review
will not result in a material adjustment in HCP’s revenue and profitability, even if the information HCP submitted to the plan is accurate and supportable. Since the CMS rules, regulations, and statements regarding this audit program are still
not well defined and, in some cases, have not been published in final form, there is also a risk that CMS may adopt new rules and regulations that are inconsistent with their existing rules, regulations, and statements.
Separately, as described in further detail below, on March 13, 2015, JSA HealthCare Corporation (JSA), a subsidiary of HCP, received a
subpoena from the Office of the Inspector General of the U.S. Department of Health and Human Services that relates, in part, to risk adjustment practices and data.
S-19
A failure to accurately estimate incurred but not reported medical expense could adversely affect
HCP’s profitability.
Patient care costs include estimates of future medical claims that have been incurred by the patient but
for which the provider has not yet billed HCP. These claim estimates are made utilizing actuarial methods and are continually evaluated and adjusted by management, based upon HCP’s historical claims experience and other factors, including an
independent assessment by a nationally recognized actuarial firm. Adjustments, if necessary, are made to medical claims expense and capitated revenues when the assumptions used to determine HCP’s claims liability changes and when actual claim
costs are ultimately determined.
Due to the inherent uncertainties associated with the factors used in these estimates and changes in the
patterns and rates of medical utilization, materially different amounts could be reported in HCP’s financial statements for a particular period under different conditions or using different, but still reasonable, assumptions. It is possible
that HCP’s estimates of this type of claim may be inadequate in the future. In such event, HCP’s results of operations could be adversely impacted. Further, the inability to estimate these claims accurately may also affect HCP’s
ability to take timely corrective actions, further exacerbating the extent of any adverse effect on HCP’s results.
HCP faces certain
competitive threats which could reduce HCP’s profitability and increase competition for patients.
HCP faces certain
competitive threats based on certain features of the Medicare programs, including the following:
| |
• |
|
As a result of the direct and indirect impacts of the Health Reform Acts, many Medicare beneficiaries may decide that an original FFS Medicare program is more attractive than a Medicare Advantage plan. As a result,
enrollment in the health plans HCP serves may decrease. |
| |
• |
|
Managed care companies offer alternative products such as regional preferred provider organizations (PPOs) and private FFS plans. Medicare PPOs and private FFS plans allow their patients more flexibility in selecting
physicians than Medicare Advantage health plans, which typically require patients to coordinate care with a primary care physician. The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 has encouraged the creation of regional
PPOs through various incentives, including certain risk corridors, or cost reimbursement provisions, a stabilization fund for incentive payments, and special payments to hospitals not otherwise contracted with a Medicare Advantage plan that treat
regional plan enrollees. The formation of regional Medicare PPOs and private FFS plans may affect HCP’s relative attractiveness to existing and potential Medicare patients in their service areas. |
| |
• |
|
The payments for the local and regional Medicare Advantage plans are based on a competitive bidding process that may indirectly cause a decrease in the amount of the PMPM fee or result in an increase in benefits
offered. |
| |
• |
|
The annual enrollment process and subsequent lock-in provisions of the Health Reform Acts may adversely affect HCP’s level of revenue growth as it will limit the ability of a health plan to market to and enroll new
Medicare beneficiaries in its established service areas outside of the annual enrollment period. |
| |
• |
|
CMS allows Medicare beneficiaries who are enrolled in a Medicare Advantage plan with a quality rating of 4.5 stars or less to enroll in a 5-star rated Medicare Advantage plan at any time during the benefit year.
Therefore, HCP may face a competitive disadvantage in recruiting and retaining Medicare beneficiaries. |
In addition to the
competitive threats intrinsic to the Medicare programs, competition among health plans and among healthcare providers may also have a negative impact on HCP’s profitability. For example, due to the
S-20
large population of Medicare beneficiaries, HCP’s Existing Geographic Regions have become increasingly attractive to health plans that may compete with HCP. HCP may not be able to continue
to compete profitably in the healthcare industry if additional competitors enter the same market. If HCP cannot compete profitably, the ability of HCP to compete with other service providers that contract with competing health plans may be
substantially impaired.
HCP competes directly with various regional and local companies that provide similar services in HCP’s
Existing Geographic Regions. HCP’s competitors vary in size and scope and in terms of products and services offered. HCP believes that some of its competitors and potential competitors may be significantly larger than HCP and have greater
financial, sales, marketing, and other resources. Furthermore, it is HCP’s belief that some of its competitors may make strategic acquisitions or establish cooperative relationships among themselves.
A disruption in HCP’s healthcare provider networks could have an adverse effect on HCP’s operations and profitability.
In any particular service area, healthcare providers or provider networks could refuse to contract with HCP, demand higher payments, or take
other actions that could result in higher healthcare costs, disruption of benefits to HCP’s members, or difficulty in meeting applicable regulatory or accreditation requirements. In some service areas, healthcare providers or provider networks
may have significant market positions. If healthcare providers or provider networks refuse to contract with HCP, use their market position to negotiate favorable contracts, or place HCP at a competitive disadvantage, then HCP’s ability to
market or to be profitable in those service areas could be adversely affected. HCP’s provider networks could also be disrupted by the financial insolvency of a large provider group. Any disruption in HCP’s provider networks could result in
a loss of members or higher healthcare costs.
HCP’s revenues and profits could be diminished if HCP fails to retain and attract the services
of key primary care physicians.
Key primary care physicians with large patient enrollment could retire, become disabled, terminate
their provider contracts, get lured away by a competing independent physician association or medical group, or otherwise become unable or unwilling to continue practicing medicine or contracting with HCP or its associated physicians, physician
groups, or IPAs. In addition, HCP’s associated physicians, physician groups and IPAs could view the business model as unfavorable or unattractive to such providers, which could cause such associated physicians, physician groups or IPAs to
terminate their relationships with HCP. Moreover, given limitations relating to the enforcement of post-termination noncompetition covenants in California, it would be difficult to restrict a primary care physician from competing with HCP’s
associated physicians, physician groups, or IPAs. As a result, members who have been served by such physicians could choose to enroll with competitors’ physician organizations or could seek medical care elsewhere, which could reduce HCP’s
revenues and profits. Moreover, HCP may not be able to attract new physicians to replace the services of terminating physicians or to service its growing membership.
Participation in ACO programs is new and subject to federal regulation, supervision, and evolving regulatory developments and may result in financial
liability.
The Health Reform Acts established Medicare Shared Savings Programs (MSSP) for ACOs, which took effect in January 2012.
Under the MSSP, eligible organizations are accountable for the quality, cost and overall care of Medicare beneficiaries assigned to an ACO and may be eligible to share in any savings below a specified benchmark amount. The Secretary of HHS is also
authorized, but not required, to use capitation payment models with ACOs. HCP has formed an MSSP ACO through a subsidiary and is evaluating whether to participate in more ACOs in the future. The continued development and expansion of ACOs will have
an uncertain impact on HCP’s revenue and profitability.
S-21
The ACO programs are new and therefore operational and regulatory guidance is limited. It is
possible that the operations of HCP’s subsidiary ACO may not fully comply with current or future regulations and guidelines applicable to ACOs, may not achieve quality targets or cost savings, or may not attract or retain sufficient physicians
or patients to allow HCP to meet its objectives. Additionally, poor performance could put the HCP ACO at financial risk with a potential obligation to CMS. Traditionally, other than FFS billing by the medical clinics and healthcare facilities
operated by HCP, HCP has not directly contracted with CMS and has not operated any health plans or provider sponsored networks. Therefore, HCP may not have the necessary experience, systems, or compliance to successfully achieve a positive return on
its investment in the ACO or to avoid financial or regulatory liability. HCP believes that its historical experience with fully delegated managed care will be applicable to operation of its subsidiary ACO, but there can be no such assurance.
California hospitals may terminate their agreements with HealthCare Partners Affiliates Medical Group (HCPAMG) or reduce the fees they pay to HCP.
In California, HCPAMG maintains significant hospital arrangements designed to facilitate the provision of coordinated hospital
care with those services provided to members by HCPAMG and its associated physicians, physician groups, and IPAs. Through contractual arrangements with certain key hospitals, HCPAMG provides utilization review, quality assurance, and other
management services related to the provision of patient care services to members by the contracted hospitals and downstream hospital contractors. In the event that any one of these key hospital agreements is amended in a financially unfavorable
manner or is otherwise terminated, such events could have a material adverse effect on HCP’s financial condition, and results of operations.
HCP’s professional liability and other insurance coverage may not be adequate to cover HCP’s potential liabilities.
HCP maintains primary professional liability insurance and other insurance coverage through California Medical Group Insurance Company, Risk
Retention Group, an Arizona corporation in which HCP is a majority owner, and through excess coverage contracted through third-party insurers. HCP believes such insurance is adequate based on its review of what it believes to be all applicable
factors, including industry standards. Nonetheless, potential liabilities may not be covered by insurance, insurers may dispute coverage or may be unable to meet their obligations, the amount of insurance coverage and/or related reserves may be
inadequate, or the amount of any HCP self-insured retention may be substantial. There can be no assurances that HCP will be able to obtain insurance coverage in the future, or that insurance will continue to be available on a cost-effective basis,
if at all. Moreover, even if claims brought against HCP are unsuccessful or without merit, HCP would have to defend itself against such claims. The defense of any such actions may be time-consuming and costly and may distract HCP management’s
attention. As a result, HCP may incur significant expenses and may be unable to effectively operate its business.
Changes in the rates or methods
of third-party reimbursements may adversely affect HCP operations.
Any negative changes in governmental capitation or FFS rates or
methods of reimbursement for the services HCP provides could have a significant adverse impact on HCP’s revenue and financial results. Since governmental healthcare programs generally reimburse on a fee schedule basis rather than on a
charge-related basis, HCP generally cannot increase its revenues from these programs by increasing the amount it charges for its services. Moreover, if HCP’s costs increase, HCP may not be able to recover its increased costs from these
programs. Government and private payors have taken and may continue to take steps to control the cost, eligibility for, use, and delivery of healthcare services due to budgetary constraints, and cost containment pressures as well as other financial
issues. HCP believes that these trends in cost containment will continue. These cost containment measures, and other market changes in non-governmental insurance plans have generally restricted HCP’s ability to recover, or shift to
non-governmental payors, any increased costs that HCP experiences. HCP’s business and financial operations may be materially affected by these cost containment measures, and other market changes.
S-22
HCP’s business model depends on numerous complex management information systems and any failure to
successfully maintain these systems or implement new systems could materially harm HCP’s operations and result in potential violations of healthcare laws and regulations.
HCP depends on a complex, specialized, and integrated management information system and standardized procedures for operational and financial
information, as well as for HCP’s billing operations. HCP may experience unanticipated delays, complications, or expenses in implementing, integrating, and operating these integrated systems. Moreover, HCP may be unable to enhance its existing
management information system or implement new management information systems where necessary. HCP’s management information system may require modifications, improvements, or replacements that may require both substantial expenditures as well
as interruptions in operations. HCP’s ability to implement and operate its integrated systems is subject to the availability of information technology and skilled personnel to assist HCP in creating and maintaining these systems.
HCP’s failure to successfully implement and maintain all of its systems could have a material adverse effect on its business, financial
condition, and results of operations. For example, HCP’s failure to successfully operate its billing systems could lead to potential violations of healthcare laws and regulations. If HCP is unable to handle its claims volume, or if HCP is
unable to pay claims timely, HCP may become subject to a health plan’s corrective action plan or de-delegation until the problem is corrected, and/or termination of the health plan’s agreement with HCP. This could have a material adverse
effect on HCP’s operations and profitability. In addition, if HCP’s claims processing system is unable to process claims accurately, the data HCP uses for its incurred but not reported (IBNR) estimates could be incomplete and HCP’s
ability to accurately estimate claims liabilities and establish adequate reserves could be adversely affected. Finally, if HCP’s management information systems are unable to function in compliance with applicable state or federal rules and
regulations, including, without limitation, medical information confidentiality laws such as HIPAA, possible penalties and fines due to this lack of compliance could have a material adverse effect on HCP’s financial condition, and results of
operations.
HCP may be impacted by eligibility changes to government and private insurance programs.
Due to potential decreased availability of healthcare through private employers, the number of patients who are uninsured or participate in
governmental programs may increase. The Health Reform Acts have increased the participation of individuals in the Medicaid program in states that elected to participate in the expanded Medicaid coverage. A shift in payor mix from managed care and
other private payors to government payors as well as an increase in the number of uninsured patients may result in a reduction in the rates of reimbursement to HCP or an increase in uncollectible receivables or uncompensated care, with a
corresponding decrease in net revenue. Changes in the eligibility requirements for governmental programs such as the Medicaid program under the Health Reform Acts and state decisions on whether to participate in the expansion of such programs also
could increase the number of patients who participate in such programs and the number of uninsured patients. Even for those patients who remain in private insurance plans, changes to those plans could increase patient financial responsibility,
resulting in a greater risk of uncollectible receivables. These factors and events could have a material adverse effect on HCP’s business, financial condition, and results of operations.
Negative publicity regarding the managed healthcare industry generally or HCP in particular could adversely affect HCP’s results of operations or
business.
Negative publicity regarding the managed healthcare industry generally, the Medicare Advantage program or HCP in
particular, may result in increased regulation and legislative review of industry practices that further increase HCP’s costs of doing business and adversely affect HCP’s results of operations or business by:
| |
• |
|
requiring HCP to change its products and services; |
| |
• |
|
increasing the regulatory, including compliance, burdens under which HCP operates, which, in turn, may negatively impact the manner in which HCP provides services and increase HCP’s costs of providing services;
|
S-23
| |
• |
|
adversely affecting HCP’s ability to market its products or services through the imposition of further regulatory restrictions regarding the manner in which plans and providers market to Medicare Advantage
enrollees; or |
| |
• |
|
adversely affecting HCP’s ability to attract and retain members. |
Risk factors related to our overall
business:
We are the subject of a number of investigations by the federal government and two private civil suits, any of which could result in
substantial penalties or awards against us, the imposition of certain obligations on our practices and procedures, exclusion from future participation in the Medicare, Medicaid and other federal healthcare programs and possible criminal penalties.
We are the subject of a number of investigations by the federal government. We have received subpoenas or other requests for
documents from the federal government in connection with the Vainer private civil suit, the Swoben private civil suit, the 2011 U.S. Attorney Medicaid investigation, the 2015 U.S. Attorney Transportation Investigation and the JSA investigation
described below.
In each of the Vainer and Swoben private civil suits, a relator filed a complaint against us in federal court under
the qui tam provisions of the False Claims Act (FCA) (and in the Swoben matter, provisions of the California False Claims Act, as well) and pursued the claims independently after the government declined to intervene. With regard to
the Vanier private civil suit, the parties are engaged in active litigation. The parties in that suit completed discovery in early 2014; however, in August 2014, the court granted relators’ motion for sanctions and reopened discovery on a
limited basis. The court in Vainer is considering the plaintiffs’ request for further sanctions, which could result in a range of outcomes from no other sanctions to plaintiffs’ request to strike our answer. Certain of these sanctions
could materially adversely impact our ability to defend the case. We can make no assurances as to the time or resources that will be needed to devote to this litigation. Further, while we cannot predict the ultimate outcome of this case, if the case
is resolved in favor of the plaintiffs, its resolution could have a material adverse effect on our earnings and cash flows. We recently commenced settlement discussions with the plaintiffs in Vainer. We expect to accrue an estimated loss contingency
reserve of $250 million related to this matter. Negotiations are ongoing and we can make no assurances as to whether the Vainer suit will settle and, if it does settle, whether it will settle for an amount higher than the current reserve. With
regard to the Swoben private civil suit, in July 2013, the court granted HCP’s motion and dismissed with prejudice all of the claims in the Third Amended Complaint, and in October 2013 the plaintiff filed an appeal of the dismissal, which is
currently pending. (See Note 17 to the consolidated financial statements included in our Annual Report on Form 10-K and subsequent filings for additional details regarding these and other matters).
Additionally, on March 13, 2015, JSA HealthCare Corporation (JSA), a subsidiary of HCP, received a subpoena from the Office of Inspector
General, U.S. Department of Health and Human Services. We have been advised by an attorney with the Civil Division of the United States Department of Justice in Washington, D.C., that the subpoena relates to an ongoing civil investigation concerning
Medicare Advantage service providers’ risk adjustment practices and data, including identification and verification of patient diagnoses and factors used in making the diagnoses. The subpoena requests documents and information for the period
from January 1, 2008 through December 31, 2013, for certain Medicare Advantage plans for which JSA provided services. It also requests information regarding JSA’s communications about patient diagnoses as they relate to certain
Medicare Advantage plans generally, and more specifically as related to two Florida physicians with whom JSA previously contracted. We intend to cooperate with the government’s investigation. In that regard, we intend to meet with
representatives of the government to discuss the scope of the subpoena and the production of responsive documents.
Responding to
subpoenas, investigations and civil suits as well as defending ourselves in such matters will continue to require management’s attention and we will continue to incur significant legal expense. Any negative findings or certain terms and
conditions that we might agree to accept as part of a negotiated resolution could result in substantial financial penalties or awards against or substantial payments made by us, the imposition of
S-24
certain obligations on our practices and procedures, exclusion from future participation in the Medicare and Medicaid programs and, in certain cases, criminal penalties. It is possible that
criminal proceedings may be initiated against us in connection with investigations by the federal government. To our knowledge, no proceedings have been initiated by the federal government against us at this time. At this time, we cannot predict the
ultimate outcome of these inquiries, or the potential outcome of the claims in relators’ civil suits (except as described above), or the potential range of damages, if any.
Disruptions in federal government operations and funding create uncertainty in our industry and could have a material adverse effect on our revenues,
earnings and cash flows and otherwise adversely affect our financial condition.
A substantial portion of our revenues is dependent
on federal healthcare program reimbursement, and any disruptions in federal government operations could have a material adverse effect on our revenues, earnings and cash flows. If the U.S. government defaults on its debt, there could be broad
macroeconomic effects that could raise our cost of borrowing funds, and delay or prevent our future growth and expansion. Any future federal government shutdown, U.S. government default on its debt and/or failure of the U.S. government to enact
annual appropriations could have a material adverse effect on our revenues, earnings and cash flows. Additionally, disruptions in federal government operations may negatively impact regulatory approvals and guidance that are important to our
operations, and create uncertainty about the pace of upcoming healthcare regulatory developments.
Changes in CMS diagnosis and inpatient procedure
coding require us to make modifications to processes and information systems, which could result in significant development costs and which if unsuccessful could adversely affect our revenues, earnings and cash flows.
CMS has mandated the use of new patient codes for reporting medical diagnosis and inpatient procedures, referred to as ICD-10, which requires
all providers, payors, clearinghouses, and billing services to utilize ICD-10 when submitting claims for payment. ICD-10 will affect diagnosis and inpatient procedure coding for everyone covered by HIPAA, not just those who submit Medicare or
Medicaid claims. Claims for services provided on or after the date that CMS sets must use ICD-10 for medical diagnosis and inpatient procedures or they will not be paid. We anticipate that if our services, processes or information systems or those
of our payors do not comply with ICD-10 requirements at any future date, it could potentially delay or even reduce reimbursement payments to us. These delays or reductions could negatively impact our revenues, earnings and cash flows.
While Congress voted to delay the ICD-10 implementation deadline until no earlier than October 1, 2015, CMS has the authority to delay
implementation even further, which leads to uncertainty about when ICD-10 will be mandated. Such uncertainty could lead to additional costs of running both ICD-9 and ICD-10 systems, which could negatively impact our revenues, earnings and cash
flows.
Federal and state privacy and information security laws are complex, and if we fail to comply with applicable laws, regulations and
standards, including with respect to third-party service providers that utilize sensitive personal information on our behalf, or if we fail to properly maintain the integrity of our data, protect our proprietary rights to our systems, or defend
against cybersecurity attacks, we may be subject to government or private actions due to privacy and security breaches, and our business, reputation, results of operations, financial position and cash flows could be materially and adversely
affected.
We must comply with numerous federal and state laws and regulations governing the collection, dissemination, access,
use, security and privacy of protected health information (PHI), including HIPAA and its implementing privacy and security regulations, as amended by the federal HITECH Act and collectively referred to as HIPAA. If we fail to comply with applicable
privacy and security laws, regulations and standards, including with respect to third-party service providers that utilize sensitive personal information, including PHI, on our behalf, properly maintain the integrity of our data, protect our
proprietary rights to our systems, or defend against cybersecurity attacks, our business, reputation, results of operations, financial position and cash flows could be materially and adversely affected.
S-25
Information security risks have significantly increased in recent years in part because of the
proliferation of new technologies, the use of the internet and telecommunications technologies to conduct our operations, and the increased sophistication and activities of organized crime, hackers, terrorists and other external parties, including
foreign state agents. Our operations rely on the secure processing, transmission and storage of confidential, proprietary and other information in our computer systems and networks.
We are continuously implementing multiple layers of security measures through technology, processes, and our people; utilize current security
technologies; and our defenses are monitored and routinely tested internally and by external parties. Despite these efforts, our facilities and systems and those of our third-party service providers may be vulnerable to privacy and security
incidents; security attacks and breaches; acts of vandalism or theft; computer viruses; coordinated attacks by activist entities; emerging cybersecurity risks; misplaced or lost data; programming and/or human errors; or other similar events.
Emerging and advanced security threats, including coordinated attacks, require additional layers of security which may disrupt or impact efficiency of operations.
Any security breach involving the misappropriation, loss or other unauthorized disclosure or use of confidential information, including
protected health information, financial data, competitively sensitive information, or other proprietary data, whether by us or a third party, could have a material adverse effect on our business, reputation, financial condition, cash flows, or
results of operations. The occurrence of any of these events could result in interruptions, delays, the loss or corruption of data, cessations in the availability of systems or liability under privacy and security laws, all of which could have a
material adverse effect on our financial position and results of operations and harm our business reputation. If we are unable to protect the physical and electronic security and privacy of our databases and transactions, we could be subject to
potential liability and regulatory action, our reputation and relationships with our patients and vendors would be harmed, and our business, operations, and financial results may be materially adversely affected. Failure to adequately protect and
maintain the integrity of our information systems (including our networks) and data, or to defend against cybersecurity attacks, could subject us to monetary fines, civil suits, civil penalties or criminal sanctions and requirements to disclose the
breach publicly, and may further result in a material adverse effect on our results of operations, financial position, and cash flows.
We may
engage in acquisitions, mergers or dispositions, which may affect our results of operations, debt-to-capital ratio, capital expenditures or other aspects of our business, and if businesses we acquire have liabilities we are not aware of, we could
suffer severe consequences that would materially and adversely affect our business.
Our business strategy includes growth through
acquisitions of dialysis centers and other businesses. We may engage in acquisitions, mergers, dispositions or new business models, which may affect our results of operations, debt-to-capital ratio, capital expenditures, or other aspects of our
business. There can be no assurance that we will be able to identify suitable acquisition targets or merger partners or that, if identified, we will be able to acquire these targets on acceptable terms or agree to terms with merger partners. There
can also be no assurance that we will be successful in completing any acquisitions, mergers or dispositions that we announce, executing new business models or integrating any acquired business into our overall operations. There is no guarantee that
we will be able to operate acquired businesses successfully as stand-alone businesses, or that any such acquired business will operate profitably or will not otherwise adversely impact our results of operations. Further, we cannot be certain that
key talented individuals at the business being acquired will continue to work for us after the acquisition or that they will be able to continue to successfully manage or have adequate resources to successfully operate any acquired business.
Businesses we acquire may have unknown or contingent liabilities or liabilities that are in excess of the amounts that we originally
estimated, and may have other issues, including those related to internal controls over financial reporting or issues that could affect our ability to comply with healthcare laws and regulations and other laws applicable to our expanded business. As
a result, we cannot make any assurances that the acquisitions we
S-26
consummate will be successful. Although we generally seek indemnification from the sellers of businesses we acquire for matters that are not properly disclosed to us, we are not always
successful. In addition, even in cases where we are able to obtain indemnification, we may discover liabilities greater than the contractual limits, the amounts held in escrow for our benefit (if any), or the financial resources of the indemnifying
party. In the event that we are responsible for liabilities substantially in excess of any amounts recovered through rights to indemnification or alternative remedies that might be available to us, or any applicable insurance, we could suffer severe
consequences that would substantially reduce our earnings and cash flows or otherwise materially and adversely affect our business.
If we are not
able to continue to make acquisitions, or maintain an acceptable level of non-acquired growth, or if we face significant patient attrition to our competitors or a reduction in the number of our medical directors or associated physicians, it could
adversely affect our business.
Acquisitions, patient retention and medical director and physician retention are an important part
of our growth strategy. We face intense competition from other companies for acquisition targets. In our U.S. dialysis business, we continue to face increased competition from large and medium-sized providers which compete directly with us for
acquisition targets as well as for individual patients and medical directors. In addition, as we continue our international dialysis expansion into various international markets, we will face competition from large and medium-sized providers for
these acquisition targets as well. Because of the ease of entry into the dialysis business and the ability of physicians to be medical directors for their own centers, competition for growth in existing and expanding markets is not limited to large
competitors with substantial financial resources. Occasionally, we have experienced competition from former medical directors or referring physicians who have opened their own dialysis centers. In addition, Fresenius, our largest competitor,
manufactures a full line of dialysis supplies and equipment in addition to owning and operating dialysis centers. This may give it cost advantages over us because of its ability to manufacture its own products. If we are not able to continue to make
acquisitions, continue to maintain acceptable levels of non-acquired growth, or if we face significant patient attrition to our competitors or a reduction in the number of our medical directors or associated physicians, it could adversely affect our
business.
HCP operates in a different line of business from our historical business. We may face challenges managing HCP as a new business and may
not realize anticipated benefits.
As a result of the HCP transaction, we are now significantly engaged in a new line of business.
We may not have the expertise, experience, and resources to pursue all of our businesses at once, and we may be unable to successfully operate all businesses in the combined company. The administration of HCP will require implementation of
appropriate operations, management, and financial reporting systems and controls. We may experience difficulties in effectively implementing these and other systems. The management of HCP will require the focused attention of our management team,
including a significant commitment of its time and resources. The need for management to focus on these matters could have a material and adverse impact on our revenues and operating results. If the HCP operations are less profitable than we
currently anticipate or we do not have the experience, the appropriate expertise, or the resources to pursue all businesses in the combined company, the results of operations and financial condition may be materially and adversely affected.
If we fail to successfully maintain an effective internal control over financial reporting, the integrity of our financial reporting could be
compromised which could result in a material adverse effect on our reported financial results.
The integration of HCP into our
internal control over financial reporting has required and will continue to require significant time and resources from our management and other personnel and will increase our compliance costs. Failure to maintain an effective internal control
environment could have a material adverse effect on our ability to accurately report our financial results and the market’s perception of our business and our stock price.
S-27
The trading prices of our debt securities, including the notes offered hereby, may be affected by factors
different from those affecting our debt securities prior to consummation of the HCP transaction.
Our historical business differs
substantially from that of HCP. Accordingly, the results of operations of the combined company and the trading prices of our debt securities, including the notes offered hereby, may be affected by factors different from those that previously
affected the independent results of operations of each of the Company and HCP.
Expansion of our operations to and offering our services in markets
outside of the U.S. subjects us to political, economical, legal, operational and other risks that could adversely affect our business, results of operations and cash flows.
We are continuing an expansion of our operations by offering our services outside of the U.S., which increases our exposure to the inherent
risks of doing business in international markets. Depending on the market, these risks include, without limitation, those relating to:
| |
• |
|
changes in the local economic environment; |
| |
• |
|
political instability, armed conflicts or terrorism; |
| |
• |
|
intellectual property legal protections and remedies; |
| |
• |
|
procedures and actions affecting approval, production, pricing, reimbursement and marketing of products and services; |
| |
• |
|
repatriating or moving to other countries cash generated or held abroad, including considerations relating to tax-efficiencies and changes in tax laws; |
| |
• |
|
lack of reliable legal systems which may affect our ability to enforce contractual rights; |
| |
• |
|
changes in local laws or regulations; |
| |
• |
|
potentially longer ramp-up times for starting up new operations and for payment and collection cycles; |
| |
• |
|
financial and operational, and information technology systems integration; and |
| |
• |
|
failure to comply with U.S. or local laws that prohibit us or our intermediaries from making improper payments to foreign officials for the purpose of obtaining or retaining business. |
Additionally, some factors that will be critical to the success of our international business and operations will be different than those
affecting our domestic business and operations. For example, conducting international operations requires us to devote significant management resources to implement our controls and systems in new markets, to comply with local laws and regulations
and to overcome the numerous new challenges inherent in managing international operations, including those based on differing languages, cultures and regulatory environments, and those related to the timely hiring, integration and retention of a
sufficient number of skilled personnel to carry out operations in an environment with which we are not familiar.
We anticipate expanding
our international operations through acquisitions of varying sizes or through organic growth, which could increase these risks. Additionally, though we might invest material amounts of capital and incur significant costs in connection with the
growth and development of our international operations, there is no assurance that we will be able to operate them profitably anytime soon, if at all. As a result, we would expect these costs to be dilutive to our earnings over the next several
years as we start-up or acquire new operations.
S-28
These risks could have a material adverse effect on our financial condition, results of
operations and cash flows.
The level of our current and future debt could have an adverse impact on our business and our ability to generate cash
to service our indebtedness depends on many factors beyond our control.
We have substantial debt outstanding, we incurred a
substantial amount of additional debt in connection with the HCP transaction and we may incur additional indebtedness in the future.
As
of December 31, 2014, after giving effect to the issuance of the notes offered hereby and the application of a portion of the estimated net proceeds therefrom to repurchase and/or redeem the outstanding 2020 Notes and to pay fees and expenses
related to this offering and the Offer as if they had occurred on that date, we would have had approximately $8.995 billion of outstanding debt, excluding the debt discount associated with our Term Loan B and outstanding undrawn letters of
credit, on our consolidated balance sheet, and approximately $905 million of available unused borrowing capacity under the revolving portion of our senior secured credit facilities (after giving effect to outstanding undrawn letters of credit
of approximately $95 million).
Our substantial indebtedness could have important consequences to you. For example, it could:
| |
• |
|
make it difficult for us to make payments on our debt securities, including the notes; |
| |
• |
|
increase our vulnerability to general adverse economic and industry conditions; |
| |
• |
|
require us to dedicate a substantial portion of our cash flow from operations to payments on our indebtedness, thereby reducing the availability of our cash flow to fund working capital, capital expenditures,
acquisitions and investments and other general corporate purposes; |
| |
• |
|
limit our flexibility in planning for, or reacting to, changes in our business and the markets in which we operate; |
| |
• |
|
expose us to interest rate volatility that could adversely affect our earnings and cash flow and our ability to service our indebtedness; |
| |
• |
|
place us at a competitive disadvantage compared to our competitors that have less debt; and |
| |
• |
|
limit our ability to borrow additional funds. |
In addition, we may incur substantial
additional indebtedness in the future. The terms of the indentures governing the notes and our existing senior notes and the agreement governing our senior secured credit facilities will allow us to incur substantial additional debt. If new debt is
added to current debt levels, the related risks described above could intensify.
Our ability to make payments on our indebtedness,
including the notes, and to fund planned capital expenditures and expansion efforts, including any strategic acquisitions we may make in the future, will depend on our ability to generate cash. This, to a certain extent, is subject to general
economic, financial, competitive, regulatory and other factors that are beyond our control.
We cannot provide assurance that our business
will generate sufficient cash flow from operations in the future or that future borrowings will be available to us in an amount sufficient to enable us to service our indebtedness or to fund other liquidity needs. If we are unable to generate
sufficient funds to service our outstanding indebtedness, we may be required to refinance, restructure, or otherwise amend some or all of such obligations, sell assets, or raise additional cash through the sale of our equity. We cannot make any
assurances that we would be able to obtain such refinancing on terms as favorable as our existing financing terms or that such restructuring activities, sales of assets, or issuances of equity can be accomplished or, if accomplished, would raise
sufficient funds to meet these obligations.
S-29
The borrowings under our senior secured credit facilities are guaranteed by a substantial portion
of our direct and indirect wholly-owned domestic subsidiaries and are secured by a substantial portion of DaVita HealthCare Partners Inc.’s and its subsidiaries’ assets.
We may be subject to liability claims for damages and other expenses not covered by insurance that could reduce our earnings and cash flows.
Our operations and how we manage the Company may subject the Company, as well as its officers and directors to whom the Company
owes certain defense and indemnity obligations, to litigation and liability for damages. Our business, profitability and growth prospects could suffer if we face negative publicity or we pay damages or defense costs in connection with a claim that
is outside the scope or limits of coverage of any applicable insurance coverage, including claims related to adverse patient events, contractual disputes, professional and general liability, and directors’ and officers’ duties. In
addition, we have received several notices of claims from commercial payors and other third parties related to our historical billing practices and the historical billing practices of the centers acquired from Gambro Healthcare and other matters
related to their settlement agreement with the Department of Justice. Although the ultimate outcome of these claims cannot be predicted, an adverse result with respect to one or more of these claims could have a material adverse effect on our
financial condition, results of operations, and cash flows. We currently maintain insurance coverage for those risks we deem are appropriate to insure against and make determinations about whether to self-insure as to other risks or layers of
coverage. However, a successful claim, including a professional liability, malpractice or negligence claim which is in excess of any applicable insurance coverage, or that is subject to our self-insurance retentions, could have a material adverse
effect on our earnings and cash flows.
In addition, if our costs of insurance and claims increase, then our earnings could decline.
Market rates for insurance premiums and deductibles have been steadily increasing. Our earnings and cash flows could be materially and adversely affected by any of the following:
| |
• |
|
the collapse or insolvency of our insurance carriers; |
| |
• |
|
further increases in premiums and deductibles; |
| |
• |
|
increases in the number of liability claims against us or the cost of settling or trying cases related to those claims; or |
| |
• |
|
an inability to obtain one or more types of insurance on acceptable terms, if at all. |
S-30
DaVita (NYSE:DVA)
Historical Stock Chart
From Mar 2024 to Apr 2024
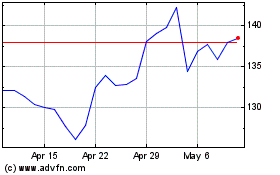
DaVita (NYSE:DVA)
Historical Stock Chart
From Apr 2023 to Apr 2024