UnitedHealth Reports Profit Decline Amid Exchange Weakness--3rd Update
January 19 2016 - 11:16AM
Dow Jones News
By Lisa Beilfuss and Anna Wilde Mathews
UnitedHealth Group Inc. said profit declined in its latest
quarter as the biggest U.S. health insurer booked charges related
to its health-care exchange segment and a Medicaid contract,
offsetting strength in its health-services unit.
The Minnetonka, Minn., company in November said it had suffered
major losses on policies sold on the Affordable Care Act's
exchanges in 2015, and warned that those losses would continue this
year. Exchanges represent a small share of UnitedHealth's overall
membership and revenue, but UnitedHealth said it booked a $245
million loss in the fourth quarter for advance recognition of 2016
losses.
The $245 million loss was larger than the approximately $200
million the company had earlier said it planned to set aside, and
UnitedHealth said it is now expecting 2016 losses on its ACA
products of more than $500 million, up from around $475 million for
2015.
The company attributed the increase largely to growing
enrollment, which is expanding despite its efforts to dampen
sign-ups. UnitedHealth said it has around 700,000 enrollees through
the ACA exchanges, up from about 500,000 at the end of 2015, and it
expects the total to grow to slightly under 800,000 by the end of
the open-enrollment period.
However, UnitedHealth said its efforts to alleviate losses,
including higher premiums and product tweaks such as withdrawing
rich "platinum" plans, had squeezed its loss margin to the "low
double digits" from the midteens earlier. UnitedHealth Group Chief
Executive Stephen J. Hemsley said the loss assumptions reflected
"prudence," as the company ensured it had "covered ourselves
appropriately."
UnitedHealth said the exchanges contributed to the company's
consolidated medical-care ratio--the amount of premiums used to pay
patient medical costs--rising to 82.7% in the fourth quarter, up
from 80.9% in the third quarter and 80.1% in fourth quarter 2014.
In addition, the company set aside $95 million in reserves for
expected losses stemming from a state Medicaid contract.
Ongoing strength in UnitedHealth's health-services arm Optum
helped counter weakness in its exchange business. Revenue there
jumped 70% to $21.9 billion, representing half of the company's top
line, powered by Optum's prescription segment. The business has
been buoyed by UnitedHealth's acquisition of pharmacy-benefit
manager Catamaran Corp., which closed in July.
During the quarter, UnitedHealth added 315,000 customers,
bringing its tally to roughly 13.5 million.
Overall, the company reported a profit of $1.22 billion, or
$1.26 a share, down from $1.51 billion, or $1.55, a year earlier.
Excluding certain items, per-share profit declined to $1.40 from
$1.64.
Revenue increased 30% to $43.60. Analysts expected earnings of
$1.38 a share on revenue of $43.23 billion.
UnitedHealth, which kicks off earnings reports for health
insurers, backed its outlook for 2016, still projecting $7.60 to
$7.80 in adjusted earnings per share and at least $180 billion in
revenue. Analysts are looking for $7.72 in adjusted per-share
profit and $181.37 billion in sales for the year.
In its Optum business, the company said it expects to fill 1
billion adjusted prescriptions this year, up from 778 million in
2015.
Shares in the company, down 9.5% over the past three months
through Friday, rose 3.3% to $112.90 in morning trading.
Write to Lisa Beilfuss at lisa.beilfuss@wsj.com and Anna Wilde
Mathews at anna.mathews@wsj.com
(END) Dow Jones Newswires
January 19, 2016 11:01 ET (16:01 GMT)
Copyright (c) 2016 Dow Jones & Company, Inc.
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Mar 2024 to Apr 2024
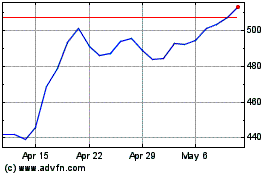
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Apr 2023 to Apr 2024
