Specialty Drugs Force High Medicare Out-Of-Pocket Costs
March 01 2010 - 7:52PM
Dow Jones News
Specialty prescription drugs are taking a big bite out of
seniors' wallets, according to the Government Accountability
Office.
A report issued by the GAO states that high-cost
drugs--classified as drugs with a monthly cost of at least $500--in
recent years have imposed far higher out-of-pocket costs for
seniors on Medicare who used them than for those who didn't. The
report focused on a class of drugs known as "specialty-tier," which
tend to be the most expensive drugs on the market.
The drugs are designated by private prescription-drug plans that
participate in the Medicare Part D program. Because of a "doughnut
hole" in Part D coverage, which forces seniors to pay the entire
cost for prescription drugs within a certain cost range, the price
of the specialty-tier drugs can weigh heavily on Part D
enrollees.
The gap in coverage under which enrollees have to pay the full
price of drugs takes effect between the cost range of $2,700 and
$6,154 per year. Above $6,154 in drug costs, Medicare pays the
majority of the cost of purchasing drugs, which is considered
catastrophic coverage.
According to the GAO, seniors using specialty-tier drugs reached
the catastrophic-coverage threshold 55% of the time, while those
who did not reached the threshold only 8% of the time. According to
report, some drug plans said that the high costs came in part
because Centers for Medicare and Medicaid Services limited their
ability to exclude drugs from their plans in favor of
less-expensive competing drugs.
Examples of specialty-tier drugs cited by GAO included Enbrel,
which is manufactured by Pfizer Inc. (PFE) for the treatment of
rheumatoid arthritis, and Gleevec, which is manufactured by
Novartis AG (NVS) for treatment of leukemia.
Rep. Pete Stark (D., Calif.), who heads the House Ways and Means
Health Subcommittee, said in a statement that "the best way to
reduce out-of-pocket drug costs is to provide coverage through the
doughnut hole, so that seniors aren't ever paying 100 percent of
their drug costs." Democrats have pushed to close the doughnut hole
as part of health-care overhaul legislation.
The Pharmaceutical Care Management Association, a trade group
that represents pharmacy benefit managers, said the report shows a
need to allow more generic versions of biologic drugs to come on to
the market. The group's members include companies such as Medco
Health Solutions Inc. (MHS) and CVS Caremark Corp (CVS).
"Generic competition lowers costs because it gives patients the
power to choose and gives manufacturers an incentive to reduce
prices," the group said in a statement.
-By Patrick Yoest, Dow Jones Newswires; 202-862-3554;
patrick.yoest@dowjones.com
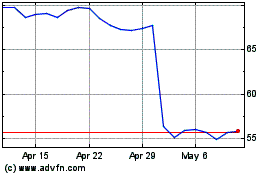
CVS Health (NYSE:CVS)
Historical Stock Chart
From Mar 2024 to Apr 2024
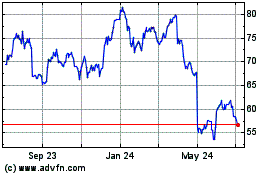
CVS Health (NYSE:CVS)
Historical Stock Chart
From Apr 2023 to Apr 2024