Teleflex Launches Triple-Lumen Version of Unique ARROW® PICC with Chlorag+ard® Technology
February 19 2015 - 5:30PM
Business Wire
World’s First Antimicrobial and
Antithrombogenic
Peripherally Inserted Central Catheter (PICC)
Now Available in Complete Portfolio of Single-, Double- and
Triple-Lumen Formats and Related Kits
Teleflex Incorporated (NYSE:TFX), a leading global provider of
medical devices for critical care and surgery, announced the launch
of the triple-lumen ARROW® PICC with Chlorag+ard® Technology. This
completes the Company’s portfolio of PICCs with the unique and
groundbreaking Chlorag+ard® Technology.
“With the completion of our ARROW® PICC with Chlorag+ard®
Technology portfolio, Teleflex can now help provide the benefits of
Chlorag+ard® Technology to all patients with PICCs, whether they
require a single-, double-, or triple-lumen device,” said Jay
White, President, Vascular Division of Teleflex. “Because ARROW®
PICCs with Chlorag+ard® Technology are both antimicrobial and
antithrombogenic, they provide an extra measure of protection
against thrombosis, occlusion, intimal hyperplasia and infection.
That is a crucial advantage at a time when many hospitals still
struggle to minimize these potentially deadly and costly
complications. Additionally, as house-wide reporting takes effect
as part of the Affordable Care Act in 2015, Chlorag+ard®
Technology’s proven ability to reduce PICC-related CLABSI will be
important for hospitals to consider.”
Pressure-injectable ARROW® PICCs with Chlorag+ard® Technology
are the world’s first FDA-cleared central venous catheters to
significantly reduce the risk of central line-associated
bloodstream infections (CLABSI) and PICC-related vessel thrombosis,
compared to traditional uncoated catheters.1 They are also the only
PICCs in the IV catheter marketplace that have received FDA 510(k)
clearance for both broad-spectrum antimicrobial and
antithrombogenic protection.
Hospitals and clinicians have increasingly focused on reducing
CLABSI and catheter-related vessel thrombosis when inserting PICCs,
which are widely used in acute-care and long-term care settings.
CLABSI is fatal in 12%-25% of cases concerning critically ill
patients without cancer and 31%-36% of cases involving critically
ill patients with cancer.2 PICC-related vessel thrombosis can lead
to a CLABSI and also cause other serious complications such as deep
vein thrombosis (DVT) and pulmonary embolism.3
In addition to CLABSI and thrombosis, the ARROW® PICC with
Chlorag+ard® Technology protects against thrombotic, intraluminal
catheter occlusion, the most common non-infectious complication in
the long-term use of central lines.4 Occlusions can delay patient
therapy and also require the use of expensive de-clotting
agents.
Chlorag+ard® Technology uses a proprietary process to chemically
bond chlorhexidine to both the internal and external surfaces of
the catheter. The chlorhexidine-bonded surfaces, which provide a
controlled release of the broad-spectrum antimicrobial, are the key
to the PICC’s antimicrobial and antithrombogenic benefits.
Studies have shown that the risk of PICC-related infections is
similar to the widely recognized risk of bloodstream infections
with central venous catheters (CVCs). In fact, certain patient
populations may be at higher risk for PICC-related infections.5,6,7
Published rates of PICC- associated symptomatic upper extremity
vessel thrombosis vary from 3.0% - 7.8%8,9, while asymptomatic
rates are as high as 38.5%.10
The impact of these complications on the healthcare economy is
also significant, with the average cost of care for upper extremity
vessel thrombosis exceeding $11,000 per incident11 and the cost of
care for CLABSIs exceeding $45,000 per incident.12
The ARROW® PICC with Chlorag+ard® Technology has been the
subject of two recently published studies that documented
substantial reduction in CLABSIs. Both studies appeared in the
Journal of the Association for Vascular Access (JAVA).13,14
The FDA clearance for ARROW® PICCs with Chlorag+ard® Technology
states that these IV catheters provide less thrombus accumulation
for at least 30 days. In Vitro data establishes that the device
provides 99.99% colonization reduction against gram + and gram -
bacteria and fungi for at least 30 days.15
Consideration of antimicrobial catheters is supported by
multiple regulatory and clinician organizations such as the Centers
for Disease Control and Epidemiology, the Society for Health
Epidemiology of America, and the Infusion Nurses Society. Their
recommendations and guidelines generally urge consideration of
antimicrobial catheter usage if the IV catheter is expected to
dwell greater than five days and if, after successful
implementation of a comprehensive strategy to reduce rates of
CLABSI, the CLABSI rate is not decreasing.16,17
Additional information may be found at www.chloragard.com.
About Teleflex Incorporated
Teleflex is a leading global provider of specialty medical
devices for a range of procedures in critical care and surgery. Our
mission is to provide solutions that enable healthcare providers to
improve outcomes and enhance patient and provider safety.
Headquartered in Wayne, PA, Teleflex employs approximately 11,500
and serves healthcare providers worldwide. Additional information
about Teleflex can be obtained from the company's website at
teleflex.com.
Forward-Looking Statements
Any statements contained in this press release that do not
describe historical facts may constitute forward-looking
statements. Any forward-looking statements contained herein are
based on our management's current beliefs and expectations, but are
subject to a number of risks, uncertainties and changes in
circumstances, which may cause actual results or company actions to
differ materially from what is expressed or implied by these
statements. These risks and uncertainties are identified and
described in more detail in our filings with the Securities and
Exchange Commission, including our Annual Report on Form 10-K.
Teleflex, Arrow, and Chorag+ard are trademarks or registered
trademarks of Teleflex Incorporated or its affiliates.© 2015
Teleflex Incorporated. All rights reserved. MC-001026
References:
- Data on file using an intravascular
ovine model.
- Chopra V, Anand S, Krein SL, et al.
Bloodstream infection, venous thrombosis and peripherally inserted
central catheters: reappraising the evidence. Am J Med., 2012,
125(8):733-741.
- Timsit JF, Misset B, Carlet J, et al.
Central vein catheter-related thrombosis in intensive care
patients: incidence, risks factors, and relationship with
catheter-related sepsis. Chest, 1998,114:207-213.
- McKnight S. Nurse's guide to
understanding and treating thrombotic occlusion of central vascular
access devices. Medsurg Nurs, 2004, 13:377-382.
- Maki DG, Kluger DM, Crnich CJ. The risk
of bloodstream infection in adults with different intravascular
devices: a systematic review of 200 published prospective studies.
Mayo Clin Proc, 2006, 81(9):1159-1171.
- Ajenjo MC, Morley JC, Russo
AJ, et al. Peripherally inserted central venous catheter-associated
bloodstream infections in hospitalized adult patients. Infect
Control Hosp Epidemiol, 2011, 32(2):125-130.
- Donowitz GR, Maki DG, Crnich CJ et al.
Infections in the neutropenic patient — new views of an old
problem. Hematology Am Soc Hematol Educ Program. 2001;113-39.
- Evans SR, Sharp JH, Lorraine LH, et al.
Risk of symptomatic DVT associated with peripherally inserted
central catheters. Chest, 2010,138:803-810.
- Cowl CT, Weinstock
JV, Al-Jurf A, et al. Complications and cost associated with
parenteral nutrition delivered to hospitalized patients through
either subclavian or peripherally-inserted central
catheters.Clinical Nutrition, 2000, 19(4): 237-243.
- Abdullah BJ, Mohammad
N, Sangkar JV, et al. Incidence of upper limb venous
thrombosis associated with peripherally inserted central catheters
(PICC). Br J Radiol, 2005, 78(931):596-600.
- de Lissovoy G, Yusen
RD, Spiro TE, et al. Cost for inpatient care of venous
thrombosis: a trial of enoxaparin vs standard heparin. Arch Intern
Med, 2000,160(20):3160-3165.
- Zimlichman E, et al. Health
Care–Associated Infections: A Meta-analysis of Costs and Financial
Impact on the US Health Care System; JAMA Intern
Med.2013;173(22):2039-2046.
- Tavianini HD, Deacon V, Negrete J, et
al. Up for the challenge: eliminating peripherally inserted central
catheter infections in a complex patient population. J Vasc Access,
2014,19(3): 159–164.
- Rutkoff GS. The influence of an
antimicrobial peripherally inserted central catheter on central
line-associated bloodstream infections in a hospital environment, J
Vasc Access, 2014,19(3):172–179.
- In vitro data on file, as compared to
uncoated PICCs, intravascular ovine model.
- O'Grady NP, Alexander M, Burns LA, et
al. Guidelines for the prevention of intravascular catheter-related
infections. Clin Infect Dis, 2011, 52(9):e162–e193.
- Infusion Nurses Society. Infusion
nursing standards of practice. J Infus Nurs. 2011, 34(1S):
S1-S110.
Teleflex IncorporatedJake ElguiczeTreasurer and Vice President,
Investor
Relations610-948-2836jake.elguicze@teleflex.comwww.teleflex.com
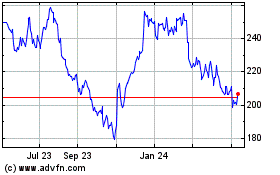
Teleflex (NYSE:TFX)
Historical Stock Chart
From Mar 2024 to Apr 2024

Teleflex (NYSE:TFX)
Historical Stock Chart
From Apr 2023 to Apr 2024