TIDMAZN
RNS Number : 0505O
AstraZeneca PLC
30 September 2019
30 September 2019 07:00 BST
Tagrisso is the only 1st-line treatment for EGFR-mutated
non-small cell lung cancer to deliver a median overall survival of
more than three years
28% of patients in the global FLAURA trial were still receiving
Tagrisso at
three years vs. 9% on either gefitinib or erlotinib
Tagrisso showed a 52% reduction in risk of central nervous
system
disease progression or death
AstraZeneca today announced overall survival (OS) results from
the Phase III FLAURA trial of Tagrisso (osimertinib) in the
1st-line treatment of adult patients with locally advanced or
metastatic epidermal growth factor receptor (EGFR)-mutated
non-small cell lung cancer (NSCLC).
Results showed a statistically significant and clinically
meaningful improvement in OS, a key secondary endpoint for Tagrisso
versus gefitinib or erlotinib, both of which were previous
standard-of-care (SoC) treatments in this setting (HR 0.799 [95%
CI, 0.641-0.997], p=0.0462).
Tagrisso delivered a median OS of 38.6 months versus 31.8 months
for the comparator arm. At three years, 28% of patients in the
Tagrisso arm and 9% of patients in the comparator arm remained on
1st-line study treatment. Tagrisso also showed a statistically
significant and clinically meaningful 52% reduction in the risk of
central nervous system (CNS) disease progression, increasing the
time patients with CNS metastases lived without CNS disease
progression or death (HR 0.48 [95% CI, 0.26-0.86], p=0.014).(1)
The results were presented at the Presidential Symposium of the
ESMO (European Society for Medical Oncology) 2019 Congress in
Barcelona, Spain (Abstract #LBA5_PR).
José Baselga, Executive Vice President, Oncology R&D said:
"Tagrisso has set a new benchmark in EGFR-mutated non-small cell
lung cancer by demonstrating a median overall survival of more than
three years. We have not before seen survival benefits of this
magnitude in any global Phase III trial with any such therapy. The
ground-breaking data reaffirm the benefit of using Tagrisso first
and further support its use as the 1st-line standard of care in
this setting."
Dr Suresh S. Ramalingam, Principal Investigator of the FLAURA
trial from Winship Cancer Institute of Emory University, Atlanta,
US, said: "The results of the FLAURA trial provide further evidence
to support the role of osimertinib as the preferred 1st-line
therapy option for patients with EGFR-mutated non-small cell lung
cancer. It is highly noteworthy that 28% of patients are still
being treated with 1st-line osimertinib at three years versus 9% on
either gefitinib or erlotinib."
Summary of FLAURA results
Tagrisso EGFR-tyrosine kinase inhibitors (TKI)
(n=279) (gefitinib or erlotinib)
(n=277)
Progression-free survival (PFS) (primary endpoint)(i)
======================================================
Median in months 18.9 10.2 months
(95% CI) (15.2, 21.4) (9.6, 11.1)
=============== =====================================
Hazard ratio 0.46
(95% CI) (0.37, 0.57)
======================================================
p-value p < 0.0001
======================================================
OS (secondary endpoint)(i)
======================================================
Hazard ratio 0.799
(95% CI) (0.641-0.997)
======================================================
p-value p = 0.0462(ii)
======================================================
Median in months 38.6 31.8
(95% CI) (34.5-41.8) (26.6-36.0)
=============== =====================================
Survival at 12 months 89.1% 82.5%
(95% CI) (84.8-92.2) (77.4-86.6)
=============== =====================================
Survival at 24 months 74.2% 58.9%
(95% CI) (68.6-79.0) (52.7-64.6)
=============== =====================================
Survival at 36 months 53.7% 44.1%
(95% CI) (47.5-59.5) (38.0-50.1)
=============== =====================================
CNS PFS (secondary endpoint)(i,1)
======================================================
Hazard ratio 0.48
(95% CI) (0.26-0.86)
======================================================
p-value p = 0.014
======================================================
Median in months Not reached 13.9
(95% CI) (16.5-NC)(iii) (8.3-NC)(iii)
=============== =====================================
Time to first subsequent therapy or death (TFST) (exploratory
endpoint)(i)
======================================================
Hazard ratio 0.48
(95% CI) (0.39-0.58)
======================================================
Number (%) of patients with events 69.5% 87.4%
=============== =====================================
Median in months 25.5 13.7
(95% CI) (22.0, 29.1) (12.3, 15.7)
=============== =====================================
Time to second subsequent therapy or death (TSST) (exploratory
endpoint)(i)
-------------------------------------------------------------- ------------------------------------------------------
Hazard ratio 0.69
(95% CI) (0.56-0.84)
======================================================
Number (%) of patients with events 64.5% 73.3%
-------------------------------------------------------------- --------------- -------------------------------------
Median in months 31.1 23.4
(95% CI) (28.8, 35.9) (20.0, 25.6)
-------------------------------------------------------------- --------------- -------------------------------------
Patients remaining on initial study treatment
-------------------------------------------------------------- ------------------------------------------------------
12 months 69.5% 47.3%
-------------------------------------------------------------- --------------- -------------------------------------
24 months 42.3% 16.2%
=============== =====================================
36 months 28.0% 9.4%
=============== =====================================
(I) The data cut-off date was 25 June 2019 (OS, TFST, TSST) and
12 June 2017 (PFS, CNS PFS)
(ii) Criteria for statistical significance at the final analysis
of OS was a p-value of less than 0.0495 (determined by O'Brien-
Fleming approach)
(iii) NC=Not Calculable
In the FLAURA trial, the safety and tolerability of Tagrisso was
consistent with its established profile. Tagrisso was generally
well tolerated, with Grade 3 or higher adverse events (AEs)
occurring in 42% of patients taking Tagrisso versus 47% in the
comparator arm. The most common AEs in patients treated with
Tagrisso were diarrhoea (60%), rash (59%), nail toxicity (39%), dry
skin (38%), stomatitis (29%), fatigue (21%) and decreased appetite
(20%). Despite almost twice the length of therapy, fewer patients
experienced a grade 3 or higher AE (42% vs. 47%) or discontinued
due to AEs (15% vs. 18%).
The FLAURA trial met its primary endpoint in July 2017, showing
a statistically significant and clinically meaningful improvement
in PFS, increasing the time patients lived without disease
progression or death from any cause.
Tagrisso is currently approved in 78 countries, including the
US, Japan, China and the EU, for 1st-line EGFR-mutated (EGFRm)
metastatic NSCLC.
About lung cancer
Lung cancer is the leading cause of cancer death among both men
and women, accounting for about one-fifth of all cancer deaths,
more than breast, prostate and colorectal cancers combined.(2) Lung
cancer is broadly split into NSCLC and small cell lung cancer
(SCLC), with 80-85% classified as NSCLC.(3) Approximately 10-15% of
NSCLC patients in the US and Europe, and 30-40% of patients in Asia
have EGFRm NSCLC.(4-6) These patients are particularly sensitive to
treatment with EGFR-TKIs which block the cell-signalling pathways
that drive the growth of tumour cells. Approximately 25% of
patients with EGFRm NSCLC have brain metastases at diagnosis,
increasing to approximately 40% within two years of diagnosis.(7)
The presence of brain metastases often reduces median survival to
less than eight months.(8)
About Tagrisso
Tagrisso (osimertinib) is a third-generation, irreversible
EGFR-TKI designed to inhibit both EGFR-sensitising and EGFR
T790M-resistance mutations, with clinical activity against CNS
metastases. Tagrisso 40mg and 80mg once-daily oral tablets have now
received approval in more than 75 countries, including the US,
Japan, China and the EU, for 1st-line EGFRm advanced NSCLC, and in
more than 85 countries, including the US, Japan, China and the EU,
for 2nd-line use in patients with EGFR T790M mutation-positive
advanced NSCLC. Tagrisso is also being developed in the adjuvant
setting (ADAURA trial), in the locally-advanced unresectable
setting (LAURA), in combination with chemotherapy (FLAURA2) in the
metastatic setting, and with potential new medicines to address
resistance to EGFR-TKIs (SAVANNAH, ORCHARD).
About FLAURA
The FLAURA trial assessed the efficacy and safety of Tagrisso
80mg orally once daily versus comparator EGFR-TKIs (either
gefitinib [250mg orally, once daily] or erlotinib [150mg orally,
once daily]) in previously-untreated patients with locally-advanced
or metastatic EGFRm NSCLC. The trial was double-blinded and
randomised, with 556 patients across 29 countries.
About AstraZeneca in lung cancer
AstraZeneca has a comprehensive portfolio of approved and
potential new medicines in late-stage clinical development for the
treatment of different forms of lung cancer spanning several stages
of disease, lines of therapy and modes of action. We aim to address
the unmet needs of patients with EGFR-mutated tumours as a genetic
driver of disease, which occur in 10-15% of NSCLC patients in the
US and EU and 30-40% of NSCLC patients in Asia, with our approved
medicines Iressa (gefitinib) and Tagrisso, and ongoing Phase III
trials ADAURA, LAURA and FLAURA2 as well as the Phase II
combination trials SAVANNAH and ORCHARD.(4-6)
Our extensive late-stage Immuno-Oncology programme focuses on
lung cancer patients without a targetable genetic mutation which
represents approximately three-quarters of all patients with lung
cancer.(9) Imfinzi (durvalumab), an anti-PDL1 antibody, is in
development for patients with advanced disease (Phase III trials
POSEIDON, PEARL, and CASPIAN) and for patients in earlier stages of
disease including potentially-curative settings (Phase III trials
AEGEAN, PACIFIC-2, ADRIATIC, ADJUVANT BR.31, PACIFIC-4, and
PACIFIC-5) both as monotherapy and in combination with tremelimumab
and/or chemotherapy.
About AstraZeneca in oncology
AstraZeneca has a deep-rooted heritage in oncology and offers a
quickly-growing portfolio of new medicines that has the potential
to transform patients' lives and the Company's future. With at
least six new medicines to be launched between 2014 and 2020, and a
broad pipeline of small molecules and biologics in development, the
Company is committed to advance oncology as a key growth driver for
AstraZeneca focused on lung, ovarian, breast and blood cancers. In
addition to AstraZeneca's main capabilities, the Company is
actively pursuing innovative partnerships and investments that
accelerate the delivery of our strategy, as illustrated by the
investment in Acerta Pharma in haematology.
By harnessing the power of four scientific platforms -
Immuno-Oncology, Tumour Drivers and Resistance, DNA Damage Response
and Antibody Drug Conjugates - and by championing the development
of personalised combinations, AstraZeneca has the vision to
redefine cancer treatment and, one day, eliminate cancer as a cause
of death.
About AstraZeneca
AstraZeneca is a global, science-led biopharmaceutical company
that focuses on the discovery, development and commercialisation of
prescription medicines, primarily for the treatment of diseases in
three therapy areas - Oncology, Cardiovascular, Renal and
Metabolism (CVRM), and Respiratory. AstraZeneca operates in over
100 countries and its innovative medicines are used by millions of
patients worldwide. Please visit astrazeneca.com and follow us on
Twitter @AstraZeneca.
Media Relations
Gonzalo Viña +44 203 749 5916
Rob Skelding Oncology +44 203 749 5821
Rebecca Einhorn Oncology +1 301 518 4122
Matt Kent BioPharmaceuticals +44 203 749 5906
Jennifer Hursit Other +44 203 749 5762
Christina Malmberg Hägerstrand Sweden +46 8 552 53 106
Michele Meixell US +1 302 885 2677
Investor Relations
Thomas Kudsk Larsen +44 203 749 5712
Henry Wheeler Oncology +44 203 749 5797
Christer Gruvris BioPharmaceuticals (CV, metabolism) +44 203 749 5711
Nick Stone BioPharmaceuticals (respiratory, renal) +44 203 749 5716
Josie Afolabi Other medicines +44 203 749 5631
Craig Marks Finance, fixed income +44 7881 615 764
Jennifer Kretzmann Corporate access, retail investors +44 203 749 5824
US toll-free +1 866 381 72 77
References
1. Vansteenkiste J, et al. CNS Response to Osimertinib vs
Standard of Care (SoC) EGFR-TKI as First-line Therapy in Patients
(pts) with EGFR-TKI Sensitising Mutation (EGFRm)-positive Advanced
Non-Small Cell Lung Cancer (NSCLC): Data from the FLAURA Study.
Annals of Oncology. 2017:28(10);189 [Accessed September 2019].
2. World Health Organization. International Agency for Research
on Cancer. Globocan Worldwide Fact Sheet 2018. Available at
http://globocan.iarc.fr/Pages/fact_sheets_population.aspx [Accessed
September 2019].
3. LUNGevity Foundation. Types of Lung Cancer. Available at
https://www.lungevity.org/about-lung-cancer/lung-cancer-101/types-of-lung-cancer
[Accessed September 2019].
4. Szumera-Ciećkiewicz A, et al. EGFR Mutation Testing on
Cytological and Histological Samples in Non-Small Cell Lung Cancer:
a Polish, Single Institution Study and Systematic Review of
European Incidence. Int J Clin Exp Pathol. 2013:6;2800-12 [Accessed
September 2019].
5. Keedy VL, et al. American Society of Clinical Oncology
Provisional Clinical Opinion: Epidermal Growth Factor Receptor
(EGFR) Mutation Testing for Patients with Advanced Non-Small-Cell
Lung Cancer Considering First-Line EGFR Tyrosine Kinase Inhibitor
Therapy. J Clin Oncol. 2011:29;2121-27 [Accessed September
2019].
6. Ellison G, et al. EGFR Mutation Testing in Lung Cancer: a
Review of Available Methods and Their Use for Analysis of Tumour
Tissue and Cytology Samples. J Clin Pathol. 2013:66;79-89 [Accessed
September 2019].
7. Rangachari, et al. Brain Metastases in Patients with
EGFR-Mutated or ALK-Rearranged Non-Small-Cell Lung Cancers. Lung
Cancer. 2015;88,108-111 [Accessed September 2019].
8. Ali A, et al. Survival of Patients with Non-small-cell Lung
Cancer After a Diagnosis of Brain Metastases. Curr Oncol.
2013;20(4):e300-e306 [Accessed September 2019].
9. Pakkala, S, et al. Personalized therapy for lung cancer:
striking a moving target. JCI Insight. 2018;3(15):e120858.
Adrian Kemp
Company Secretary
AstraZeneca PLC
This information is provided by RNS, the news service of the
London Stock Exchange. RNS is approved by the Financial Conduct
Authority to act as a Primary Information Provider in the United
Kingdom. Terms and conditions relating to the use and distribution
of this information may apply. For further information, please
contact rns@lseg.com or visit www.rns.com.
END
MSCLFFSIATIAFIA
(END) Dow Jones Newswires
September 30, 2019 02:02 ET (06:02 GMT)
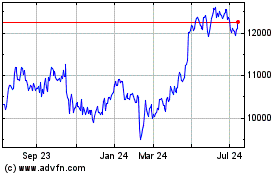
Astrazeneca (LSE:AZN)
Historical Stock Chart
From Mar 2024 to Apr 2024
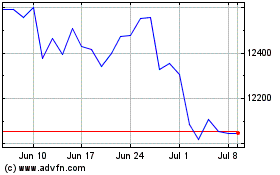
Astrazeneca (LSE:AZN)
Historical Stock Chart
From Apr 2023 to Apr 2024