OptumRx Receives Pharmacy Benefit Management Institute’s Excellence Award for Opioid Risk Management
March 05 2019 - 2:00PM
Business Wire
- Program uses comprehensive approach to
reduce inappropriate prescribing, dispensing and consumption of
prescription opioids
- Results show significant improvements
in health outcomes for patients and clients
OptumRx has received the 2019 Excellence Award for Opioid
Management Strategies from the Pharmacy Benefit Management
Institute. The award recognizes OptumRx for significantly reducing
excessive prescribing, dispensing and consumption of prescription
opioids – while delivering quality care – through its Opioid Risk
Management program, a comprehensive initiative addressing the
opioid epidemic.
This press release features multimedia. View
the full release here:
https://www.businesswire.com/news/home/20190305005755/en/
Since the program’s launch in July 2017, OptumRx has
successfully helped clients and patients balance the need for these
powerful medications with the risk of abuse and misuse.
- Reducing the opioid supply:
Clients who adopted short-acting opioid utilization management
criteria experienced a 31 percent decrease in opioid prescription
volume and a 42 percent decrease in the total morphine milligram
equivalent (MME) exposure among patients receiving opioid
prescriptions.
- Decreasing progression from acute to
chronic use: Clients who adopted first-fill dose and duration
limits for patients not receiving opioids on a daily basis showed a
50 percent lower likelihood of these patients progressing from
short-term acute use to longer-term chronic opioid use after the
first fill.
- Improving clinical best
practices: In line with the Centers for Disease Control and
Prevention’s recommended best practices for prescribers, 96 percent
of opioid prescriptions among Optum customers who adopted the
program were in full alignment with dosage and duration guidelines,
vs. 55 percent national average.
“Using advanced data analytics and evidence-based clinical
strategies, we are mitigating opioid misuse and abuse before it
starts, while supporting people who may be battling dependency and
addiction issues, as well as those in recovery,” said David
Calabrese, chief pharmacy officer at OptumRx. “We are honored to be
recognized by PBMI for the positive impact we are having on the
patients and clients we serve.”
The OptumRx Opioid Risk Management program extends beyond what
traditional, stand-alone pharmacy benefit organizations can address
by targeting five key factors contributing to this complex health
care crisis, including:
- Prevention and education:
Educating all stakeholders regarding risks, proper dosing/duration,
storage, safer treatment alternatives and proper disposal.
- Minimizing early exposure:
Limiting opioid dose and duration of therapy at first fill.
- Reducing inappropriate supply:
Applying protocols to reduce excessive dosing, limit unnecessary
extensions, mitigate abuse and decrease exposure to harmful drug
combinations.
- Treating at-risk and
high-risk members: Preventing progression to chronic use, abuse
and dependence through intensive, multidimensional program
efforts.
- Supporting chronic populations and
recovery: Guiding patients with current or previous overdose
experience/dependence issues/opioid use disorder and providing
advanced patient monitoring, support and relapse prevention.
“OptumRx’s Opioid Risk Management program stands apart because
of its dual focus on reducing both the consumption and prescription
of opioids, enabling the company to achieve unparalleled results on
both fronts,” said Jane Lutz, executive director of PBMI. “Knowing
that OptumRx is continually updating the program to advance
positive results for its members, we look forward to the work that
is to come.”
OptumRx is continuing to expand its efforts to curb the rise of
opioid abuse through a variety of new components recently launched
and in development, including:
- More aggressive first-fill dose and
duration limits (3 days; 50mg/day) for children and young
adults;
- Decreased opioid dispensing through
OptumRx Home Delivery Pharmacy to a maximum of 30-day supply only,
which helps reduce excess supply and supports safe and appropriate
opioid use; and
- Adherence monitoring and intervention
for patients on medication assisted therapy.
For more information on OptumRx’s Opioid Risk Management
program, visit our resource page.
About OptumRxOptumRx is a pharmacy care services company
helping clients and more than 65 million members achieve better
health outcomes and lower overall costs through innovative
prescription drug benefit services, including network claims
processing, clinical programs, formulary management and specialty
pharmacy care. Through expertise, flexible technology and a network
of over 67,000 community pharmacies and state-of-the-art home
delivery pharmacies, OptumRx is putting patients at the center of
the pharmacy experience and making health care more connected and
less fragmented — ensuring patients get the right medication at the
right time at the best cost. OptumRx is part of Optum®, a leading
information and technology-enabled health services business
dedicated to making the health system work better for everyone.
Optum is part of UnitedHealth Group (NYSE:UNH). For more
information, visit optum.com/optumrx or follow @OptumRx on
Twitter.
About PBMIThe Pharmacy Benefit Management Institute
(PBMI) is the nation’s leading provider of research and education
that informs, advises, and influences the industry on topics
related to drug cost management. PBMI offers research,
continuing education, and web resources to help all critical
stakeholders work better together to optimize the overall value of
drug benefit programs. Learn more at www.pbmi.com.
Click here to subscribe to Mobile Alerts for UnitedHealth
Group.
View source
version on businesswire.com: https://www.businesswire.com/news/home/20190305005755/en/
OptumJennifer StathamTel: (952)
205-7747jennifer.statham@optum.com
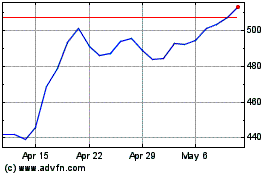
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Mar 2024 to Apr 2024
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Apr 2023 to Apr 2024
