Employers Struggle To Make a Dent in Health Costs
February 01 2018 - 12:02PM
Dow Jones News
By Anna Wilde Mathews and Joseph Walker
The planned venture by Amazon.com Inc., Berkshire Hathaway Inc.
and JPMorgan Chase & Co. to overhaul their workers' health care
follows years of similar efforts by employers to change a complex
and entrenched industry, with mixed success.
The three big companies shook up health-care firms' shares
Tuesday by saying they will form a not-for-profit company to reduce
costs and improve the health-care experience of hundreds of
thousands of U.S. employees. People with knowledge of the matter
said nothing had been decided beyond creating the new company, but
worries about the potential threat pushed down shares of insurers
and pharmacy benefit managers.
Yet even with its high-profile backers, the project will face
many of the same barriers as did previous employer efforts to come
together to reform the giant U.S. health-care sector, which
represents about 17.9% of the gross domestic product.
"This is not a new idea," said Lonny Reisman, a former executive
at Aetna Inc. who helped create an employer coalition in the 1990s
that crafted deals with health-maintenance organizations. Do
employer groups "have enough clout to actually change the nature of
health-care delivery and pricing?" he said. "I don't think they've
been very successful."
Earlier employer alliances have mostly been able to point to
incremental gains, such as cheaper pharmacy-benefit rates for
members or improvements in public quality measures of health-care
providers and health insurers. They haven't managed "in a wholesale
way to transform an industry, which is what these guys are trying
to do," said Jim Winkler, a senior vice president at consulting
firm Aon PLC. "It is really hard to do."
The Health Transformation Alliance, founded in 2016, is perhaps
the highest-profile existing employer effort, with 46 members
including American Express Co., Johnson & Johnson and Macy's
Inc. -- as well as JPMorgan and Berkshire's BNSF Railway Co.
A JPMorgan spokesman said the bank, after joining weeks ago,
hasn't yet joined any of the alliance's initiatives. A BNSF
spokesman didn't respond to a request for comment.
The alliance this year began contracting with two
pharmacy-benefit managers, or PBMs, to provide lower prices and
more transparency on fees and rebates. This year, 21 companies are
participating in the contracts, and four more are slated to join
next year, alliance CEO Robert Andrews said in an interview. The
PBM contracts will save the 21 current participants at least $600
million over three years compared with their previous deals, he
estimated.
The alliance is also contracting with health-care providers in
certain markets to care for employees with diabetes, hip and knee
replacements and lower back pain. The contracts are supposed to pay
doctors based on how well they meet targets such as quick recovery
times.
In June, the alliance began an effort to meld member companies'
health-claims data into International Business Machines Corp.'s
Watson software.
It may take more radical steps in the future, such as forming
its own PBM if its current pharmacy-benefits contracts don't meet
its goals. "Who can deliver that is still an open question, whether
it's our own PBM or another existing organization," Mr. Andrews
said. "We're looking at every option on the table."
Many large employers have joined purchasing coalitions focused
on pharmacy benefits, some formed by big consultants such as Aon
and Willis Towers Watson. These coalitions typically negotiate
deals with PBMs on behalf of their members. The members get "better
pricing and a packaged set of services," said Julie Stone, a
practice leader at Willis Towers Watson, due partly to "the size
the coalition has grown to and the leverage" it generates with
suppliers.
One challenge for employers seeking to make large-scale changes
is that health-care markets are fractured and vary widely by
market. Even large national employers often have limited
populations in a particular location.
"You need critical mass locally to leverage a pricing
advantage," said Brian Marcotte, chief executive of the National
Business Group on Health, which offers advice and research for
employers but doesn't seek to purchase services for its members.
"You still need the delivery system to provide the care."
Health-care vendors can fight back against employers'
cooperative work. An employer group, the Pharmaceutical Coalition,
in 2015 dissolved a drug-pricing transparency initiative after PBMs
started requiring the employers to sign "very tight nondisclosure
agreements," said Amanda H. Beck, a spokeswoman for the HR Policy
Association, an umbrella group that spearheaded the coalition. The
group's members, which included Caterpillar Inc., had aimed to
create stricter standards for pharmacy-benefit contracting, such as
sharing all discounts and rebates with coalition members.
Employers themselves also may struggle to unite, because they
often have far different cultures, employee populations and
geographies. "Employers have a very hard time coming to agreement
on the exact same contract terms," said Suzanne Delbanco, executive
director of Catalyst for Payment Reform, which is backed by
employers but doesn't negotiate contracts on their behalf. She says
her group has helped increase transparency on health-care prices
and move insurers toward new methods of paying health-care
providers.
--Emily Glazer and Nicole Friedman contributed to this
article.
(END) Dow Jones Newswires
February 01, 2018 11:47 ET (16:47 GMT)
Copyright (c) 2018 Dow Jones & Company, Inc.
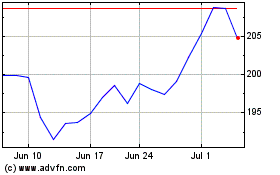
JP Morgan Chase (NYSE:JPM)
Historical Stock Chart
From Mar 2024 to Apr 2024
JP Morgan Chase (NYSE:JPM)
Historical Stock Chart
From Apr 2023 to Apr 2024
