Alliance of Companies Unveil First Steps Aimed at Cutting Health-Care Costs
March 06 2017 - 4:48PM
Dow Jones News
By Joseph Walker
A U.S. alliance formed last year by more than three dozen
companies, including American Express Co., Johnson & Johnson
and Macy's Inc., is announcing its first plans aimed at lowering
the companies' health-care spending.
The blueprint includes group contracts to purchase prescription
drugs through units of CVS Health Corp. and UnitedHealth Group
Inc.; the creation of specialized doctor networks; and a deal to
use International Business Machines Corp.'s Watson software to
analyze their health-care data.
The nonprofit group, called the Health Transformation Alliance,
says combining the negotiating heft of its 38 members allows it to
win lower prices than any individual company could alone.
Each company must still decide whether to participate in the
prescription-drug contracts, after comparing the
alliance-negotiated deals with their existing prescription
arrangements, according to the alliance.
The alliance expects at least 20 members to participate, and
estimates they will save a combined $600 million over three years
compared with their current drug-benefit contracts, says HTA Chief
Executive Robert Andrews, a former Democratic congressman who
helped write and pass President Barack Obama's Affordable Care Act.
The savings would represent 14% to 15% of total drug spending, on
median, for the employers.
HTA member companies provide health insurance to a combined six
million employees, the vast majority of them in the U.S., the
alliance says.
The effort is picking up at a time of growing employer concern
and congressional debate over rising health-care costs, which
represent about 18% of the U.S.'s gross domestic product. In 2016,
health-care spending by private businesses jumped 6.1% to $676
billion, compared with an average increase of 4.5% in government
and household spending on health-care, according to recent
estimates by the Centers for Medicare and Medicaid Services.
"This is the group that's paying the bill," says Kyu Rhee, chief
health officer at IBM, an alliance member. "We're not waiting for
the public sector to come up with the solution -- we have the
skills and expertise to do this ourselves."
Prescription-drug spending is of particular concern. Companies
hire middlemen called pharmacy-benefit managers, or PBMs, to
negotiate discounts and rebates on drug prices from pharmaceutical
companies and retail pharmacies. PBMs also try to keep costs down
by steering patients to lower-cost treatments, such as generics or
brand-name drugs with the largest rebates.
But PBMs often keep a portion of the discounts they negotiate
with drugmakers, without always divulging how much they're keeping.
The contract terms PBMs cut with employers can vary widely. By
giving all of their business to just two PBMs -- UnitedHealth's
OptumRx or CVS's Caremark -- the employers in the alliance will pay
less and receive more consistent prices from PBMs, said L. Kevin
Cox, chief human resources officer at American Express. "Everybody
thinks they get a good deal, but it's not true," Mr. Cox says.
Mr. Cox said employers would also gain more transparency into
the actual cost of drugs they purchase, because the contracts
include guaranteed rebates and the right to audit their PBMs.
However, it isn't clear how novel those arrangements are because
many PBM contracts with large employers already include those
features, says Craig Oberg, a pharmacy-benefits consultant at the
Burchfield Group.
The companies also hope to use the alliance to more directly
manage their employees' health care, including by determining the
best drugs and physicians to treat costly diseases and
conditions.
Starting next year, the alliance will contract with doctors and
other health-care providers in Phoenix, Chicago and Dallas-Fort
Worth to care for employees with diabetes, hip and knee
replacements, and lower back pain. The alliance aims to structure
the contracts, which will be negotiated and administered by
insurers Cigna Corp. and UnitedHealth, to pay doctors based on how
well they meet certain targets, such as quick recovery times,
rather than for each procedure and test they perform.
The alliance says it will also use IBM's Watson software to help
member companies choose the drugs and doctors that provide the best
value. Starting this year, IBM will feed about four years of data
from each company, including pharmacy and insurance claims, and
electronic health records, into the Watson software, which will
then make recommendations based on which drugs and doctors resulted
in the best health-care outcomes for patients. The alliance also
aims to have Watson predict which employees are likely to develop
diseases like diabetes, and to recommend treatment that can
possibly prevent the disease.
Write to Joseph Walker at joseph.walker@wsj.com
(END) Dow Jones Newswires
March 06, 2017 16:33 ET (21:33 GMT)
Copyright (c) 2017 Dow Jones & Company, Inc.
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Mar 2024 to Apr 2024
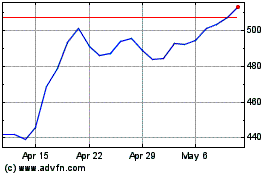
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Apr 2023 to Apr 2024
