UnitedHealth Posts Strong Results -- WSJ
July 20 2016 - 3:05AM
Dow Jones News
By Anna Wilde Mathews and Anne Steele
UnitedHealth Group Inc. on Tuesday posted a strong earnings beat
as revenue continued to surge in its pharmacy-services business,
and the biggest U.S. health insurer lifted the low end of its
profit guidance for the year.
The Minnetonka, Minn., company now expects adjusted earnings for
the year of about $7.80 to $7.95 a share, compared with its
previous forecast -- raised in April -- for $7.75 to $7.95 a
share.
But amid the positive news, the company included one ongoing
dark spot: Affordable Care Act plans, which it will almost
completely stop selling next year. The insurer booked another $200
million in full-year ACA-plan losses in the second quarter,
bringing its projected total loss for the year to about $850
million, with about $245 million of that included in 2015 results
and $605 million in 2016.
The even-bigger losses were tied to larger ACA-plan enrollment
than expected, including more limited attrition. But more than
that, costs mounted because enrollees were even sicker than
projected, with more chronic conditions than last year, adding to
the insurer's costs. Those including AIDS, hepatitis C, diabetes
and chronic obstructive pulmonary disease.
Stephen J. Hemsley, UnitedHealth Group's chief executive, said
that despite the ACA business, the medical-cost trend remained
"well-controlled and consistent with expectations," a comment
likely to reassure investors worried about a potential uptick in
health spending. Company officials said the inpatient hospital
admissions rate was lower than last year but flagged a few areas
where costs had picked up, including specialty pharmacy and
emergency- acquisition of pharmacy-benefit managerroom use.
The insurer's medical-loss ratio -- the percentage of premiums
paid in claims -- ticked up 30 basis points to 82%, but that
included more than 50 basis points of impact from the ACA
plans.
UnitedHealth's health-services arm Optum continued to show
strength, with revenue there jumping 51% to $20.6 billion,
representing about 44% of the company's top line, powered by
Optum's pharmacy-care services. The business has been buoyed by
UnitedHealth's acquisition of pharmacy-benefit manager Catamaran
Corp., which closed last July.
During the quarter, UnitedHealth added 305,000 customers,
bringing its tally to roughly 47.98 million.
In all for the June quarter, the company reported a profit of
$1.75 billion, or $1.81 a share, up from $1.59 billion, or $1.64 a
share, a year earlier. Excluding certain items, adjusted per-share
earnings rose to $1.96 from $1.73.
Revenue climbed 28% to $46.49 billion. Analysts had projected
adjusted earnings of $1.89 a share on revenue of $45.05
billion.
Shares in the company, which kicks off earnings reports for
health insurers, have risen 20% this year. In midday trading in New
York, UnitedHealth shares slid 4 cents to $140.71.
Write to Anna Wilde Mathews at anna.mathews@wsj.com and Anne
Steele at Anne.Steele@wsj.com
(END) Dow Jones Newswires
July 20, 2016 02:50 ET (06:50 GMT)
Copyright (c) 2016 Dow Jones & Company, Inc.
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Mar 2024 to Apr 2024
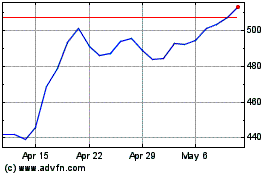
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Apr 2023 to Apr 2024
