Anthem Sees Rise in Exchange Enrollees -- WSJ
April 28 2016 - 3:03AM
Dow Jones News
By Anna Wilde Mathews and Anne Steele
Anthem Inc. said its enrollment through the Affordable Care
Act's exchanges grew more than expected in the first months of the
year. The company said it is still targeting a slim positive margin
on the business this year, striking a guardedly optimistic tone
about the marketplaces amid questions about their
sustainability.
The No. 2 U.S. health insurer said it had 975,000 exchange
enrollees at the end of the first quarter, up by around 184,000
since the end of the year. The increase drew sharp questions from
analysts after UnitedHealth Group Inc.'s recent announcement that
it would withdraw from all but a handful of the exchanges after
steepening losses.
During the company's call Wednesday to discuss first-quarter
earnings -- which, on an adjusted basis, beat analysts'
expectations -- Anthem Chief Executive Joseph R. Swedish noted that
performance on the exchanges "has lagged expectations throughout
the industry as some of our peers have recognized." He said Anthem
was being cautious in its projections and its management of pricing
and products.
Anthem believes it is "well-positioned for continued growth in
the exchange marketplace if the market stabilizes to a more
sustainable level," Mr. Swedish said, and he called for some
changes by regulators to ensure the exchange business would
work.
The company is still targeting a margin on the exchange business
for this year that is lower than its ultimate goal of 3% to 5%,
saying it likely won't achieve its 3%-to-5% aim in 2017 either, but
sees it as more doable in 2018.
Anthem has said it roughly broke even in 2015 on individual
plans -- putting it ahead of many insurers that, like UnitedHealth,
saw losses on the exchanges. The individual business has
traditionally been a more important segment for Anthem than for
some of its big national competitors. Analysts have also suggested
that as Anthem's proposed $48 billion acquisition of Cigna Corp.
remains under federal review, it may have reason to support the
exchanges, a central part of the Obama administration's signature
health law. Anthem said it was still looking to close the deal in
the second half of this year.
Much of the boosted exchange enrollment came in states where
nonprofit cooperative insurers had folded, including New York,
Colorado and Kentucky, the company said. Seeking to reassure
investors that it hadn't drawn enrollees with aggressive pricing,
the insurer emphasized that the growth came despite rates that it
said were higher than some others in those markets.
Anthem said it now expects overall revenue for the 2016 year in
the range of $81 billion to $82 billion, up from its previous
forecast for $80 billion to $81 billion. It backed its view of
adjusted earnings of greater than $10.80 a share, and Anthem
executives emphasized that one reason it kept that number constant
was the cautious stance it was taking on exchange-business
projections.
Medical enrollment grew 2.8% from a year earlier to about 39.6
million as of March 31. Revenue in the government-business segment
jumped 14% to $10.8 million.
Anthem said the growth was driven by enrollment increases in the
Medicaid business, as well as national accounts and individual
enrollment. Medicaid membership rose 7.6% from the prior-year
period to 6.05 million in the quarter. But Anthem saw a dip in
small-employer enrollment that it tied to the decision by some
states to add larger employers to the "small group" category under
the ACA.
The insurer posted a profit of $703 million, or $2.63 a share,
down from $865.2 million, or $3.09 a share, a year earlier. On an
adjusted basis, leaving out costs tied to transactions and
investments, among others, earnings rose to $3.46 a share from
$3.14. Revenue climbed 6.5% to $20.29 billion.
Analysts surveyed by Thomson Reuters had forecast per-share
earnings of $3.32 on revenue of $19.86 billion.
Anthem's medical-loss ratio -- the share of premiums used to pay
patient medical costs -- was 81.8% in the first quarter, up from
80.2% a year earlier. The climb was largely driven by the extra
calendar day in the quarter, a higher ratio in the Medicaid and
individual businesses and higher membership in the Medicaid
business, which carries a higher benefit expense ratio than the
company average.
Write to Anna Wilde Mathews at anna.mathews@wsj.com and Anne
Steele at Anne.Steele@wsj.com
(END) Dow Jones Newswires
April 28, 2016 02:48 ET (06:48 GMT)
Copyright (c) 2016 Dow Jones & Company, Inc.
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Mar 2024 to Apr 2024
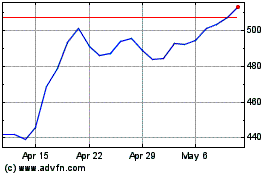
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Apr 2023 to Apr 2024
