UnitedHealth Raises Forecast for Losses on Affordable Care Act Plans--4th Update
January 19 2016 - 6:00PM
Dow Jones News
By Anna Wilde Mathews
UnitedHealth Group Inc. said its projected losses on the
Affordable Care Act exchanges for 2016 deepened, as enrollment grew
despite the company's efforts to damp sign-ups.
The biggest U.S. health insurer said it is now expecting losses
of more than $500 million on its 2016 ACA plans, compared with
previous projections that amounted to $400 million to $425 million
in losses.
UnitedHealth had taken steps to pull back on its exchange
business in anticipation of losses, including reducing marketing
and slashing commissions to health-insurance agents. But enrollment
nevertheless grew, widening the company's exposure. UnitedHealth
Group Chief Executive Stephen J. Hemsley said the new projection
reflected "prudence," as the company sought to ensure it had
covered all possible losses.
The exchange plans represent a tiny share of UnitedHealth
Group's total business. On Tuesday the company reiterated its
overall financial outlook for 2016, saying it expected $7.60 to
$7.80 in adjusted earnings per share and at least $180 billion in
revenue. Its shares closed up 3% at $112.58, as investors shrugged
off the exchange comments amid strong results elsewhere in the
company's portfolio.
But UnitedHealth's move comes amid continued worries about the
exchange business--concerns that the company jump-started in
November, when it disclosed expected 2016 losses and said it would
consider withdrawing from the health-law marketplaces, a decision
expected later this year.
Humana Inc. added another note of apprehension on Jan. 8, when
it said it too would set aside a "premium deficiency reserve" at
the end of 2015 to account for losses expected on its 2016 ACA
business. The company hasn't yet put a number on its projected
results.
The Obama administration has signaled that it will take steps to
address one of the issues that insurers have blamed for their
problems. Last week, a top federal health official said regulators
will tighten the rules for people who enroll in insurance through
the federal HealthCare.gov site outside of official enrollment
periods. Insurers have complained that the current rules can allow
people to wait to sign up when they expect to have health-care
costs.
And so far, other major insurers haven't publicly moved to
create reserves against expected 2016 exchange losses. Aetna Inc.
said last week it had losses on its exchange business in 2015 and
was aiming for a "mid-single digits" profit in 2016, but likely
wouldn't "get all the way there." Anthem Inc. said enrollment in
its individual business came in lower than expected, and it expects
its 2016 margins to be better than last year's, though still not at
its target range of 3% to 5%.
UnitedHealth said Tuesday its enrollment through the ACA
exchanges was approximately 700,000. At the end of 2015, the figure
was about 500,000. UnitedHealth said it had losses of around $475
million on its 2015 ACA-plan business.
Of its anticipated 2016 ACA-plan losses, UnitedHealth said it
had booked $245 million in 2015, as part of a "premium deficiency
reserve."
The company in November said it expected $200 million in 2016
ACA-plan losses that it would book in 2015, as well as between $200
million and $225 million that would affect its results in 2016.
Before the problems with ACA business became fully clear,
UnitedHealth had earlier decided to expand the number of markets
where it offers exchange plans for 2016, a likely reason for its
growing enrollment despite recent efforts to damp sign-ups.
In addition, UnitedHealth said its efforts to improve results on
the ACA plans, which included increased premiums and product tweaks
such as withdrawing rich "platinum" plans, had helped squeeze its
loss margin from around 15% to the "low double digits."
Overall, UnitedHealth Group reported a profit of $1.22 billion,
or $1.26 a share for the fourth quarter of 2015, down from $1.51
billion, or $1.55, a year earlier. Excluding certain items,
per-share profit declined to $1.40 from $1.64. Revenue increased
30% to $43.60 billion. Analysts expected earnings of $1.38 a share
on revenue of $43.23 billion. During the quarter, UnitedHealth
added 315,000 health-insurance customers, bringing its tally to
about 46.4 million.
The exchange business "is not something that is core to what
they do," said Chris Rigg, an analyst with Susquehanna Financial
Group, who said investors were likely also reassured that the
tweaked exchange projection was tied to enrollment, not a change in
the company's understanding of the risks.
Ana Gupte, an analyst with Leerink Partners LLC, said
UnitedHealth is offering a conservative outlook for its exchange
business that it might then beat over the course of the year.
UnitedHealth saw continuing strength from its health-services
arm, Optum, in the fourth quarter. Revenue there jumped 70% to
$21.9 billion, representing half of the company's top line, powered
by Optum's prescription segment. The business has been buoyed by
UnitedHealth's acquisition of pharmacy-benefit manager Catamaran
Corp., which closed in July.
Write to Anna Wilde Mathews at anna.mathews@wsj.com
(END) Dow Jones Newswires
January 19, 2016 17:45 ET (22:45 GMT)
Copyright (c) 2016 Dow Jones & Company, Inc.
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Mar 2024 to Apr 2024
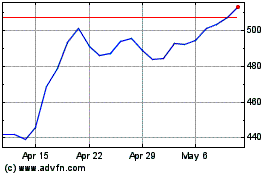
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Apr 2023 to Apr 2024
