Aetna, Anthem Say Individual Commercial Business Is On Track--2nd Update
November 20 2015 - 6:37PM
Dow Jones News
By Nathan Becker
Health insurers Aetna Inc. and Anthem Inc. on Friday said their
individual commercial businesses have performed within expectations
lately, a day after UnitedHealth Group Inc. said it was considering
exiting the Affordable Care Act's exchanges.
The statements could be a sign that big problems with business
on government exchanges aren't widespread across insurers. On
Thursday, UnitedHealth, the biggest health insurer in the U.S.,
said it has suffered deep losses on its exchange-related
business.
That announcement stoked worries about the future of the health
marketplaces that are at the center of the Obama administration's
health law.
Aetna and Anthem also backed their profit outlooks for the year
on Friday after UnitedHealth cut its view Thursday.
Still, the companies' exchange-related business isn't without
troubles--Aetna said on an earnings call earlier this month that
individual business for its public-exchange and consumer efforts
remained challenging. It plans to participate on individual
exchanges in 15 states next year, down from 17 states in 2015.
Chief Executive Mark Bertolini at the time said the 15 states
made up "a footprint that we continue to believe can drive net
membership growth."
Anthem said in October that its exchange membership declined in
the latest quarter.
Anthem Chief Executive Joseph Swedish said the company "remains
committed to enhancing access to high quality, affordable health
care for all of our members inside and outside of the insurance
exchanges and continuing our dialogue with policy makers and
regulators regarding how we can improve the stability of the
individual market."
Anthem operates in 14 exchange states.
UnitedHealth operated on individual exchanges in 23 states this
year. The company has locked in its exchange offerings for 2016,
but it is pulling back on marketing them during the current
open-enrollment period to limit membership and considering exiting
them in 2017.
Anthem and Aetna both have big merger deals on the table to be
reviewed by the government--Anthem has an agreement in place to buy
Cigna Corp., while Aetna Inc. has an agreement to buy Humana Inc.
Those moves come as the biggest insurers seek cost efficiency and
scale as the health-care landscape changes because of the
Affordable Care Act and other factors.
Molina Healthcare Inc., which is seeing profits on its exchange
business, also offered reassurance for investors nervous about the
sector after UnitedHealth's comments. Chief Executive Mario Molina
said the company wasn't seeing the issues UnitedHealth flagged. For
instance, he said, around a quarter of Molina's exchange enrollees
came in outside the annual open-enrollment period, but this group
didn't appear to be running up a notably higher health-costs tab
than others. "I don't think those patients are a whole lot
different from those who come to us during open enrollment," he
said.
UnitedHealth had said it was seeing higher costs among these
enrollees, suggesting consumers might be purchasing plans to cover
imminent medical expenses.
Dr. Molina also said he'd seen "no evidence at this point that
there is adverse selection going on within our population," meaning
that the enrollees aren't skewed toward older, sicker people who
tend to need more health care. Molina has said it has around
226,000 exchange enrollees.
Analysts have said that companies like Molina, which focus
largely on Medicaid, may have advantages that are helping them do
better in the exchange environment. Those include generally
lower-cost networks of providers, and a target population that is
relatively low-income, and thus highly subsidized by the federal
government.
Another publicly traded insurer, Centene Corp., also backed its
outlook and said its marketplace business is performing as
expected.
Ben Wakana, a spokesman for the Department of Health and Human
Services, said the statements were an indication that the overall
marketplace has strength going forward.
"It continues to grow, giving more Americans access to quality,
affordable health care, and consumers are benefiting from increased
choice and competition," Mr. Wakana said.
Anna Wilde Mathews contributed to this article
Write to Nathan Becker at nathan.becker@wsj.com
Subscribe to WSJ: http://online.wsj.com?mod=djnwires
(END) Dow Jones Newswires
November 20, 2015 18:22 ET (23:22 GMT)
Copyright (c) 2015 Dow Jones & Company, Inc.
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Mar 2024 to Apr 2024
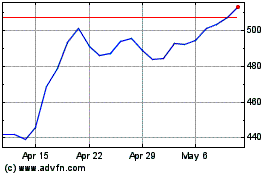
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Apr 2023 to Apr 2024
