By Peter Loftus and Anna Wilde Mathews
Health insurer Cigna Corp. will get extra price discounts from
drugmakers if new cholesterol medications don't help patients as
much as expected, a significant step in a broader push to tie the
cost of drugs to how well they work.
Such "value-based" deals are becoming more common as rising
costs spur customers to demand assurances they are getting what
they pay for. U.S. prescription spending rose 12% to nearly $425
billion in 2015, following a 13% increase in 2014, according to
research firm IMS Health.
Cigna is set to announce on Wednesday that it is the first
insurer to reach value-based contracts for an entire new class of
cholesterol drugs: Praluent, which is co-marketed by Sanofi SA and
Regeneron Pharmaceuticals Inc., and Amgen Inc.'s Repatha are the
only two cholesterol-lowering drugs known as PCSK9 inhibitors
currently on the U.S. market.
Both drugs were introduced last year to reduce levels of LDL
cholesterol, or "bad" cholesterol, beyond what can be achieved by
an older class of drugs known as statins. Reducing LDL can lower
risk of heart attacks and strokes, though Praluent and Repatha
haven't yet been proven to reduce cardiovascular risk in
trials.
Both drugs cost at least $14,000 a year, and Cigna negotiated an
undisclosed discount off the list prices.
If Cigna-insured patients who take the drugs aren't able to
reduce LDL cholesterol at least as well as what was shown in
clinical trials, the manufacturers will further discount the costs
of the drugs -- and not just for patients who didn't meet the
cholesterol goals. If the drugs meet or exceed expectations, the
original negotiated price stays, according to Cigna.
Health insurers and pharmacy-benefit managers have signed at
least a dozen such deals with drugmakers since 2014, including
Cigna, Harvard Pilgrim Health Care and Express Scripts Holding Co.,
targeting high-cost drugs in categories including cancer and
hepatitis C.
While the number of value-based deals has increased, they remain
somewhat limited in scope, and may not put a huge dent in drug
spending in the near-term, experts say. Insurers and manufacturers
say the complexity of tracking patients' health -- which falls on
the insurer -- can be a barrier, and most supply contracts still
tie payments to volume of prescriptions.
"There is a general increase in interest in exploring these
kinds of contracts, but a fair amount of caution as well, largely
because the administrative aspects tend to be quite daunting in the
short term," said Steven Pearson, president of the Institute for
Clinical and Economic Review, a Boston nonprofit that promotes
value-based drug prices.
Chris Bradbury, senior vice president for Cigna's
pharmacy-benefits business, said the deals "are protecting our
clients and customers if something doesn't work as
expected...especially for many of these medicines now that cost
thousands or tens of thousands of dollars a year."
Cigna has access to patients' cholesterol levels and will track
them over "a period of time, months and quarters," Mr. Bradbury
said, to determine whether they are meeting the targets. Cigna also
plans to track whether these patients have heart attacks and other
cardiovascular events over the long-term, but that information
doesn't determine reimbursement levels in the current contracts.
The drugs aren't currently approved to reduce the risk of
cardiovascular events.
A Cigna spokeswoman said the company can monitor patients'
adherence to prescriptions, side effects and drug interactions. The
company also can review lab results and work with customers'
doctors as needed, she said.
Joshua Ofman, senior vice president of global value and access
at Amgen, said the company has agreed to such contracts with
insurers to "address their short-term budget concerns and
real-world performance regarding Repatha." Amgen hopes the
agreement will enable patients to get access to the drug.
Sanofi and Regeneron said in a joint statement they have pursued
value-based contracts for Praluent to address insurers' "complex
needs and facilitate access for appropriate patients who require
additional treatment options to lower their bad cholesterol."
Drugmaker AstraZeneca PLC signed a deal last year with Express
Scripts to reimburse costs of the lung-cancer drug Iressa if a
patient stops treatment before the third prescription fill. And Eli
Lilly & Co. has a deal with insurer Humana Inc. that ties the
level of reimbursement for the heart drug Effient to the rate of
hospitalizations among patients who take it.
"More and more in the U.S., people are making choices between a
bag of groceries and a medicine, a copay," Paul Hudson, president
of AstraZeneca's U.S. unit, said in an interview. "The long-term
sustainability of the industry and our ability to deliver
breakthrough medicines requires us to demonstrate value."
AstraZeneca has been among the more active drugmakers pursuing
alternative payment arrangements. In addition to the Iressa
contract, AstraZeneca has a deal with University of Pittsburgh
Medical Center's regional health plan to cover a portion of the
costs of treating patients who have additional heart attacks after
taking the heart drug Brilinta, if the rate of heart attacks
exceeds a threshold. Brilinta has been shown in clinical trials to
reduce the rate of heart attacks in patients. A UPMC spokesman
declined to comment.
CVS Health Corp., the second-biggest U.S. pharmacy-benefit
manager, has also made deals that tie payment to patient
outcomes.
Alan Lotvin, executive vice president for specialty pharmacy at
CVS, said the setups can be difficult to execute because many
achievements -- such as a reduction in heart attacks and deaths for
cholesterol drugs -- can take years to become clear, while patients
may be impossible to track over time as they change insurers and
jobs.
Also, he said, drug manufacturers may have advantages in
negotiating favorable terms because they have the best data on
their products. "What we want to be sure is that we're not letting
the manufacturer use the outcomes-based arrangements to avoid the
best price on day one," Dr. Lotvin said.
Colin Wight, CEO of GalbraithWight, which advises drugmakers on
pricing strategies, says many of the value-based contracts amount
to a "fancy way of rebating." He thinks drugmakers should go
further and consider payment models used in other industries, like
software licenses. In that model, an insurer could pay a set
monthly fee to a drugmaker for as long as a patient benefits from
it, he said.
Write to Peter Loftus at peter.loftus@wsj.com and Anna Wilde
Mathews at anna.mathews@wsj.com
(END) Dow Jones Newswires
May 11, 2016 00:15 ET (04:15 GMT)
Copyright (c) 2016 Dow Jones & Company, Inc.
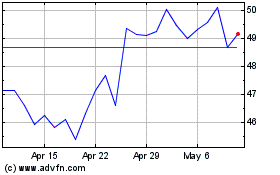
Sanofi (NASDAQ:SNY)
Historical Stock Chart
From Mar 2024 to Apr 2024
Sanofi (NASDAQ:SNY)
Historical Stock Chart
From Apr 2023 to Apr 2024
