By Peter Loftus
Patients with advanced lung cancer who took Merck & Co.'s
immune-boosting drug Keytruda as their first treatment lived longer
on average than those who received chemotherapy in a new study that
could herald a big shift in treatment of the deadliest cancer.
The finding could lead to wider use of Keytruda and help Merck
gain ground on rival Bristol-Myers Squibb Co. in the
multibillion-dollar market for new drugs that fight cancer by
harnessing patients' immune systems.
Bristol's immunotherapy Opdivo, which has so far outsold
Keytruda, failed to significantly prolong survival beyond
chemotherapy in a separate study of lung-cancer patients. Opdivo
had global sales of $1.54 billion for the first six months of 2016,
while Keytruda had sales of $563 million.
Both companies previously revealed limited results of their
respective lung-cancer studies this year; researchers presented
full results Sunday at a meeting of the European Society for
Medical Oncology in Copenhagen, and Merck's study was published
online by the New England Journal of Medicine.
Keytruda and Opdivo are approved in the U.S. to treat
lung-cancer patients whose disease has progressed after prior
chemotherapy treatment and for some other tumors. The drugs each
cost more than $12,500 a month per patient.
Lung cancer is one of the most common types of cancer and causes
the most deaths. About 224,390 new cases are expected in the U.S.
this year, while about 158,080 people are expected to die from lung
cancer, according to the American Cancer Society.
The Merck study tested Keytruda in patients with what is called
non-small cell lung cancer, the most common type of the disease,
which had spread to other parts of the body and hadn't yet been
treated. For decades, the standard first-line treatment for these
patients has been chemotherapy, but patients typically live only 12
to 14 months after starting treatment, according to Hossein
Borghaei, a lung-cancer specialist at Fox Chase Cancer Center in
Philadelphia.
About 80% of patients who took Keytruda were alive six months
after the start of treatment, compared with 72% of those on
chemotherapy.
Keytruda extended the time until death or disease progression to
a median of 10.3 months from the start of treatment, versus six
months for chemotherapy. Median overall survival of patients -- the
point at which half lived longer, half lived less -- hadn't been
reached as of the data-analysis cutoff, but typically this exceeds
progression-free survival.
Nearly 45% of patients receiving Keytruda experienced
significant tumor shrinkage, versus nearly 28% of the chemotherapy
patients.
The 305 patients in the Merck study also had a high level of a
substance known as PD-L1 in their tumors, which is believed to
enhance the effect of drugs like Keytruda. Patients with high
levels of this marker account for about 25% to 30% of all non-small
cell lung cancers, said Roger Perlmutter, head of Merck's research
and development unit, in an interview.
The study started in September 2014, and in June of this year it
was stopped early on the recommendation of an independent
monitoring committee because interim results showed that Keytruda
was superior to chemotherapy. Patients who were taking chemotherapy
were allowed to switch over to Keytruda.
Treatment-related side effects such as nausea and anemia
occurred in 73% of patients receiving Keytruda, versus 90% for
chemotherapy, though severe side effects occurred at a higher rate
among chemotherapy patients.
The Keytruda study results "may establish a new standard of
care" for first-line treatment of lung cancer patients whose tumors
have high levels of PD-L1, Bruce E. Johnson, a lung-cancer
specialist at Dana-Farber Cancer Institute in Boston, wrote in a
NEJM editorial accompanying the Keytruda results.
Merck has applied for U.S. regulatory approval to market
Keytruda as a first-line lung-cancer treatment; a decision is
expected by Dec. 24.
Bristol-Myers tested Opdivo as a first-line treatment in a
broader patient pool than Merck's study because the study also
included patients with relatively low levels of PD-L1 in their
tumors. The study found no significant difference in overall
survival or progression-free survival between the groups. Median
overall survival for Opdivo was 14.4 months, versus 13.2 months for
chemotherapy, but the difference wasn't statistically
significant.
The divergent outcomes between the Merck and Bristol studies
could reinforce an emerging practice in medicine to identify
certain biological traits of cancer and other diseases that can
help predict which patients may benefit most from a drug.
Johan Vansteenkiste, a professor of medicine at University
Hospitals Leuven in Belgium, said it is likely that Keytruda
prolonged survival because the study only enrolled patients with
high levels of PD-L1, whereas Opdivo likely failed because it also
included those with lower levels.
Bristol still hopes its immunotherapies can play a role in
first-line treatment of lung cancer. It is testing a combination of
its drugs Opdivo and Yervoy in those patients, with results
expected by early 2018, said Fouad Namouni, Bristol's head of
oncology development.
In a separate study, lung-cancer patients receiving Roche
Holding AG's immunotherapy Tecentriq after prior treatments had a
median survival of 13.8 months, compared with 9.6 months for
patients on chemotherapy. Roche has applied for U.S. regulatory
approval of Tecentriq as a second-line lung-cancer treatment, and a
decision is expected by Oct. 19.
Write to Peter Loftus at peter.loftus@wsj.com
(END) Dow Jones Newswires
October 09, 2016 02:29 ET (06:29 GMT)
Copyright (c) 2016 Dow Jones & Company, Inc.
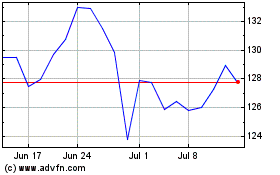
Merck (NYSE:MRK)
Historical Stock Chart
From Mar 2024 to Apr 2024
Merck (NYSE:MRK)
Historical Stock Chart
From Apr 2023 to Apr 2024
