Aetna Tops Views, Stops ACA Expansion Plans
August 02 2016 - 7:40AM
Dow Jones News
Aetna Inc. posted better-than-expected profit and revenue growth
in the most recent quarter but said it dropped plans to further
expand its Affordable Care Act business next year and will review
how it will continue—if at all—in existing states.
"While we are pleased with our overall results, in light of
updated 2016 projections for our individual products and the
significant structural challenges facing the public exchanges, we
intend to withdraw all of our 2017 public exchange expansion plans,
and are undertaking a complete evaluation of future participation
in our current 15-state footprint," said Chief Executive Mark
Bertolini.
Chief Financial Officer Shawn Guertin said Aetna delivered solid
top-line and bottom-line results in the second quarter, "despite
the challenges in our ACA compliant products."
"Our financial position, capital structure, and liquidity are
all strong, and bolstered by core businesses that continue to
produce bottom-line growth," he said.
In the June quarter, Aetna's overall medical membership fell
2.9% to 22.98 million. Medicaid membership popped 12% to 2.4
million, while Medicare Advantage membership grew 9% to 1.3
million.
Aetna's medical-benefit ratio, a key measure of the amount of
premiums used to pay patient medical costs, rose to 82.4% from
81.1%. The ratio rose more for its commercial members, to 83.4%
from 81.8%, than its government-based business, 81.4% from
80.3%.
In all for the quarter, Aetna reported earnings of $790.8
million, or $2.23 a share, up from $731.8 million, or $2.08 a
share, a year earlier.
Operating earnings rose to $2.21 a share from $2.05 a share.
Operating revenue, which excludes net realized capital gains and
losses, grew 5.1% to $15.9 billion. Analysts had forecast $2.12 a
share on $15.69 billion in revenue.
Aetna reaffirmed its 2016 operating earnings guidance for $7.90
to $8.10 a share.
Aetna in early July agreed to buy Humana Inc., part of a
rapid-fire reconfiguration of the U.S. health-insurance industry's
top ranks. The consolidation momentum is being fed by a desire to
diversify and cut costs following changes brought by the Affordable
Care Act. The deal to buy Humana would boost Hartford, Conn.-based
Aetna's Medicare business and give it scale to thrive as the
industry consolidates.
But late last month, the Justice Department filed a pair of
lawsuits in a Washington, D.C., federal court challenging Anthem
Inc.'s proposed acquisition of Cigna Corp. and Aetna's planned
combination with Humana, alleging the mergers would harm consumers,
employers and health-care providers with an unacceptable reduction
in competition.
On Tuesday, Aetna and Humana together announced they agreed to
sell separate Medicare Advantage assets to Molina Healthcare Inc.
for about $117 million in cash. The pair of transactions are
subject to the completion of the merger.
The deals give Molina about 290,000 Medicare Advantage members
in 21 states, "preserving robust competition for seniors choosing
to receive Medicare coverage through Medicare Advantage plans and
addressing a key concern of the U.S. Department of Justice in its
challenge to the Aetna-Humana transaction," the companies said in a
statement.
Mr. Bertolini said they believe these divestitures taken
together would address the Justice Department's "perceived
competitive concerns."
Humana is set to report second-quarter results tomorrow.
Shares of Aetna, inactive premarket, have risen 5.9% so far this
year.
Write to Anne Steele at Anne.Steele@wsj.com
(END) Dow Jones Newswires
August 02, 2016 07:25 ET (11:25 GMT)
Copyright (c) 2016 Dow Jones & Company, Inc.
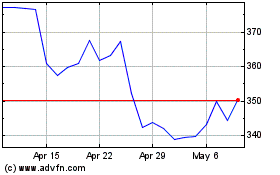
Molina Healthcare (NYSE:MOH)
Historical Stock Chart
From Mar 2024 to Apr 2024
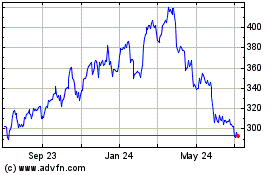
Molina Healthcare (NYSE:MOH)
Historical Stock Chart
From Apr 2023 to Apr 2024