Insurers have begun to propose big premium increases for
coverage next year under the 2010 health law, as some struggle to
make money in a market where their costs have soared.
The companies also have detailed the challenges in their
Affordable Care Act business in a round of earnings releases, the
most recent of which came on Wednesday when Humana Inc. said it
made a slim profit on individual plans in the first quarter, not
including some administrative costs, but still expects a loss for
the full year. The Louisville, Ky.-based insurer created a special
reserve fund at the end of last year to account for some expected
losses on its individual plans in 2016.
The rate picture will vary by state and by company, analysts
said, and not all insurers will need large premium increases to
bolster their financial performance. Indeed, some companies,
including Medicaid-focused insurers such as Centene Corp., have
already said plans sold through the health law's exchanges are
profitable.
Still, the analysts said, a number of insurers are likely to
seek significant hikes as they aim to cover costs that have
continued to outstrip their estimates—in some cases coming after
earlier premium increases.
The increases, along with the continued lagging results for
insurers, are a sign that the exchange business hasn't stabilized
for insurers in the first few years of the health law's full
implementation, prompting health plans to continue to push for more
changes to the law.
The health law instigated a sweeping overhaul to the way
insurance is priced and sold in the U.S. Insurers can't deny
coverage to consumers with risky medical histories, or charge them
more for plans. A number of popular insurers say the enrollees who
bought plans through the exchanges have had higher health costs
than they originally predicted—when they knew less about the impact
of the law.
"It's a pretty good bet if a plan lost money in 2016, it will
adjust pricing in 2017," said Sam Glick, a partner with consulting
firm Oliver Wyman, a unit of Marsh & McLennan Cos.
In Oregon and Virginia, the first two states to make insurers'
premium proposals for 2017 public, several big insurers are showing
how those projections bear out.
Providence Health Plan, currently the largest insurer for people
buying coverage through the Oregon health exchange, is seeking an
average increase of 29.6%.
In Virginia, where premium increases had been relatively modest
to date, Anthem Inc. is asking for an average increase of
15.8%.
Proposed average increases are just one indicator of coming
premium changes for individuals, which vary depending on the
specific plan a person buys, and they must be evaluated by
regulators before they can take effect. Increases can be blunted
for many lower-income consumers by federal subsidies that flow
directly to the insurer, offsetting the consumer's premium
bill.
Officials from the Department of Health and Human Services
emphasized the role of those subsidies and said that after
increases last year, by one estimate the average additional amount
paid by people with tax credits was only a few dollars a month.
"Averages based on proposed premium changes aren't a reliable
indicator of what typical consumers will actually pay because tax
credits reduce the cost of coverage for the vast majority of
people, shopping gives all consumers a chance to find the best
deal, and public rate review can bring down proposed increases,"
said Ben Wakana, an agency spokesman.
At the same time, the average increases present a vivid picture
of how insurers feel they are faring year-on-year.
Humana said it would make changes to its exchange offerings for
next year "to retain a viable product for individual consumers,
where feasible," and its moves may include "statewide market and
product exits both on and off exchange, service area reductions and
pricing commensurate with anticipated levels of risk by state."
Humana sold plans on exchanges in 15 states this year.
Humana's announcement follows a disclosure from UnitedHealth
Group Inc. last month that, amid deepening losses, it will next
year withdraw from all but a handful of the 34 states where it was
offering exchange plans.
Anthem and Aetna Inc. were far more upbeat about their prospects
on the health-law marketplaces in recent earnings calls, but both
have also said they aren't yet achieving their targeted margins and
aim to improve results next year.
Insurers seeking rate increases—which include several other big
plans in Oregon and Virginia—all cite the higher-than-expected
medical costs incurred by their enrollees as factors in their
decision.
In Oregon, regulators' filings show Moda Health Plan Inc., once
the largest insurer on the exchange, saying it needs to hike
premiums there by an average of 32.3%. That is coming on the heels
of an increase of around 25% last year; the insurer also said it
would stop selling individual plans in Alaska.
Kaiser Foundation Health Plan of the Northwest asked for an
increase of 14.5%, the second lowest percentage increase in
Oregon.
Oregon's insurance commissioner has the power to block proposed
premium changes, but indicated Tuesday she was looking to make sure
rates were sufficient for insurers to pay out claims as well as
affordable for consumers.
"For the next two months, we will analyze the requested rates to
ensure they adequately cover costs without being too high or too
low," said the commissioner, Laura Cali.
In Virginia, CareFirst BlueCross BlueShield's proposed average
increases are around 25%, though that number reflects the insurer's
decision to withdraw all of its lowest-premium plans, the so-called
bronze tier that has the highest cost-sharing for participants, and
the increase is around 11% for plans that have a similar level of
benefits, the insurer said.
Insurers are pointing to factors beyond medical claims that will
affect their pricing next year. Aetna has said the phasing out of
two programs designed to stabilize the Affordable Care Act
exchanges would push up the prices of exchange plans by about 6% in
2017, though the suspension of a tax on insurers will partly
mitigate that impact.
In addition, UnitedHealth's withdrawals may prod competitors to
boost rates, said Raj Bal, an insurance-industry consultant. He
suggested the remaining insurers will anticipate the effect of
signing up some of the costly enrollees that resulted in red ink
for UnitedHealth. "People will anticipate that risk will migrate to
them, and they want to price for it," he said.
Write to Louise Radnofsky at louise.radnofsky@wsj.com and Anna
Wilde Mathews at anna.mathews@wsj.com
(END) Dow Jones Newswires
May 05, 2016 08:05 ET (12:05 GMT)
Copyright (c) 2016 Dow Jones & Company, Inc.
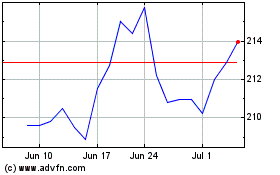
Marsh and McLennan Compa... (NYSE:MMC)
Historical Stock Chart
From Mar 2024 to Apr 2024
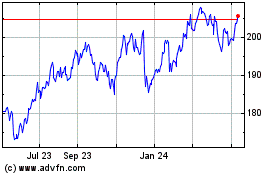
Marsh and McLennan Compa... (NYSE:MMC)
Historical Stock Chart
From Apr 2023 to Apr 2024