Aetna Not Alone In Layoffs As Other Insurers Also Pare Jobs
November 19 2009 - 3:37PM
Dow Jones News
Aetna Inc. (AET) isn't the only health insurer paring its work
force as the managed-care industry faces rising medical costs,
enrollment pressures and a competitive marketplace.
WellPoint Inc. (WLP) has eliminated jobs over the past several
weeks, although the managed-care giant isn't providing any numbers
or making any kind of layoff announcement. In addition, Cigna Corp.
(CI) has cut hundreds of jobs this year beyond those announced in
January.
The layoffs highlight the effects of the economic downturn,
which has caused the highest unemployment rate in the U.S. in 25
years, reducing the number of commercial members. The job cuts also
come ahead of anticipated government-led changes to the nation's
health-care system.
Wednesday, Aetna said it was cutting some 3.5% of its work
force--625 positions immediately and about the same number in the
first quarter of next year. These reductions are in addition to the
1,000 job eliminations, or nearly 3% of its work force, that the
Hartford insurer announced last December.
Meanwhile, Cigna has cut 1,810 jobs so far this year, a company
spokesman confirmed Thursday. That includes the 1,100 layoffs,
representing 4% of its work force, that the insurer announced in
January. During the second and third quarters, Cigna took charges
for severance tied to the elimination of 710 positions, according
to a recent Securities and Exchange Commission filing.
WellPoint, also in an SEC filing, said it made $18.5 million in
payments in the first nine months of this year related to employee
terminations and indicated it may incur charges in future periods
related to job cuts. It was unclear from the filing whether any of
these cuts were in addition to the 1,500 job eliminations,
representing 3.6% of WellPoint's work force, that the company
announced in January; those eliminations included 900 open
positions.
WellPoint has not updated layoff figures since January, although
a spokeswoman said Thursday that positions were eliminated and
added in recent weeks.
"As the economic environment changes, WellPoint reviews the size
and skills of our work force and makes adjustments as necessary.
The current economic downturn has affected our customers, and many
employers have reduced the size of their labor force in response.
This in turn has affected the membership of WellPoint's affiliated
health plans. As a result, we are examining ways we can operate
more efficiently in 2010," said spokeswoman Kristin Binns earlier
this month.
Meanwhile, WellPoint's recently announced decision to withdraw
its UniCare commercial plans from Texas and Illinois means a number
of employees in that division will lose their jobs, although the
company said it does not yet know how many of the 700 UniCare
employees will be laid off.
A staff reduction will be necessary as 360,000 affected UniCare
members switch to another insurer, as most are expected to do next
month, according to UniCare spokesman Tony Felts. The business has
about 285,000 members outside the two states, he said.
UniCare expects the first staff reductions will start in January
and continue in phases throughout 2010, depending on how many stay
with UniCare until their policies expire sometime next year, he
said.
-By Dinah Wisenberg Brin, Dow Jones Newswires; 215-656-8285;
dinah.brin@dowjones.com
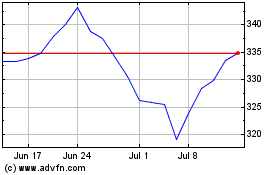
Cigna (NYSE:CI)
Historical Stock Chart
From Mar 2024 to Apr 2024
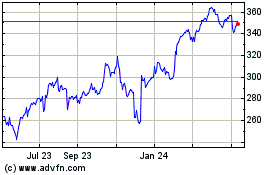
Cigna (NYSE:CI)
Historical Stock Chart
From Apr 2023 to Apr 2024