By Peter Loftus
CHICAGO -- A new study is stirring debate about whether the
benefits of cancer drugs are worth their cost, particularly as
drugmakers develop treatments that combine multiple pricey
drugs.
The study of about 4,800 women with an aggressive type of breast
cancer found that adding Roche Holding AG's drug Perjeta to the
company's older treatment Herceptin conferred a slight benefit
versus Herceptin alone, after the women had undergone surgery to
remove tumors. Some 94.1% of women receiving the combination in the
study stayed free of invasive breast cancer three years after the
start of treatment, versus 93.2% of those who received Herceptin
alone -- a difference of less than a percentage point.
That modest benefit comes at a high price: more than doubling
the one-year treatment cost to $158,000 a patient from $74,500. The
combination also had higher rates of certain side effects than
Herceptin alone, including severe diarrhea.
"The marginal improvement of adding Perjeta is tiny for the
average person, but the incremental cost is going to be
substantial," said Richard Schilsky, chief medical officer of the
American Society of Clinical Oncology, which is hosting a
conference where the study results were released Monday. He wasn't
involved in the study.
Dr. Kathy D. Miller, an oncologist at Indiana University Melvin
and Bren Simon Cancer Center in Indianapolis, wrote a critical
editorial in the New England Journal of Medicine, published online
along with the study results Monday. "The toxic effects (and cost)
are too great for too many to benefit too few," she wrote.
Roche said the benefit of Perjeta and Herceptin in the new study
could mean the difference between relapse and staying disease-free
for many women. "We see this as a very meaningful benefit," Daniel
O'Day, CEO of Roche's pharmaceutical unit, said in an interview.
The company plans to file for regulatory approval to market the
combination for patients after breast-cancer surgery, also known as
adjuvant treatment.
The finding comes as many drug companies including Roche, Merck
& Co. and AstraZeneca PLC race to test whether new combinations
of cancer drugs can improve outcomes versus single-drug therapy or
older treatments.
Last month, the Food and Drug Administration approved adding
Merck & Co.'s Keytruda, which costs $13,000 a month, to an
older combination of lung-cancer treatments that includes Eli Lilly
& Co.'s Alimta, which costs more than $5,700 for a 21-day
treatment cycle.
In 2015, the FDA approved the use of a combination of
Bristol-Myers Squibb Co.'s Yervoy and Opdivo to treat the deadly
skin cancer melanoma, based on a study showing it slowed cancer
progression better than either drug alone. The two drugs together
cost more than $250,000 for the first full year of treatment.
For one class of cancer drugs, which harness the body's immune
system to attack tumors, the number of clinical trials testing them
in combination with other drugs more than tripled to 765 from 215
in late 2015, according to a new report from industry research firm
Evaluate Ltd. Roche alone is running 45 clinical trials that test
combinations of cancer immunotherapies, said Sandra Horning, chief
medical officer of Roche's Genentech unit.
The trend concerns health insurers. UnitedHealth Group sometimes
has to pay much more for the use of cancer combination therapies
that contain pricey new brand-name drugs than it does for cheaper
combinations of generic drugs that may be just as good, Lee
Newcomer, senior vice president of oncology and genetics, said at a
panel discussion about cost at the ASCO conference.
In the study, the Perjeta-Herceptin combination had a more
pronounced benefit in a subset of women considered at higher risk
of relapse, including those with cancer that had spread to lymph
nodes, Gunter von Minckwitz, lead researcher for the study and head
of the German Breast Group, an academic alliance that runs clinical
trials, said in an interview. He said he expects health insurers
and government health programs to be more open to paying for the
combination's use in higher-risk patients.
Some doctors said they would probably avoid using the
Perjeta-Herceptin combination in patients at lower risk of relapse.
"Would I have preferred to see a higher benefit? Certainly yes,"
Eleni Andreopoulou, a breast-cancer specialist at Weill Cornell
Medicine and NewYork-Presbyterian hospital, said in an interview.
Dr. Andreopoulou, who enrolled patients in the study but wasn't a
lead researcher, called it a positive result but said she would
like to see more tests developed to predict which patients are more
likely to benefit from the combination based on biological traits
of tumors, and which aren't.
Herceptin, introduced in 1998, improved treatment of breast
tumors with high levels of the protein HER2, particularly after
surgery. Roche introduced Perjeta in 2012 to be used in combination
with Herceptin to try for an even greater benefit.
Regulators previously approved the Herceptin-Perjeta combination
to treat HER2-positive breast cancer at earlier and later stages of
development than the one in the new study: cancers that have spread
to other parts of the body, and cancers before women undergo
surgery.
Roche reported about $7 billion in global Herceptin sales last
year, and about $1.9 billion in Perjeta sales.
Write to Peter Loftus at peter.loftus@wsj.com
(END) Dow Jones Newswires
June 05, 2017 07:44 ET (11:44 GMT)
Copyright (c) 2017 Dow Jones & Company, Inc.
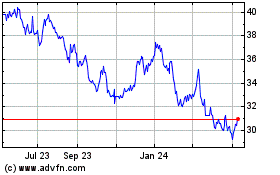
Roche (QX) (USOTC:RHHBY)
Historical Stock Chart
From Mar 2024 to Apr 2024
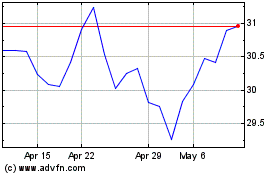
Roche (QX) (USOTC:RHHBY)
Historical Stock Chart
From Apr 2023 to Apr 2024