Showed event-free and overall survival rates
of 65.5% and 91.5%, respectively
14.2% of patients treated with
Sprycel induction therapy received stem cell transplant in first
remission
Bristol-Myers Squibb Company (NYSE:BMY) today announced data
from the phase 2 CA180-372 study in pediatric patients with newly
diagnosed Philadelphia chromosome-positive (Ph+) acute
lymphoblastic leukemia (ALL) treated with Sprycel (dasatinib) added
to a chemotherapy regimen modelled on a Berlin-Frankfurt-Munster
high-risk backbone. The combination demonstrated an event-free
survival (EFS) rate, the study’s primary endpoint, of 65.5% (95%
CI: 57.7 to 73.7), and an overall survival (OS) rate of 91.5% (95%
CI: 84.2 to 95.5) at three years. Sprycel and chemotherapy were
generally well-tolerated in pediatric Ph+ ALL patients. Results
will be presented today during an oral session (Abstract #98) at
the 2017 American Society of Hematology Annual Meeting in Atlanta,
Georgia.
“Philadelphia chromosome-positive acute lymphoblastic leukemia
remains a high-risk leukemia type,” said Stephen Hunger, MD, lead
study author, Chief of the Division of Oncology and Director of the
Center for Childhood Cancer Research at Children’s Hospital of
Philadelphia. “In this study, the addition of dasatinib to
chemotherapy in pediatric patients with Ph+ ALL yielded similar
event-free and overall survival rates to recent North American and
European pediatric Ph+ ALL trials, with a lower percentage of
patients undergoing hematopoietic stem cell transplantation in
first remission, indicating the potential of dasatinib as a new
treatment option for these patients.”
Patients treated in the study (n=106), all aged younger than 18
years, received continuous daily Sprycel beginning at day 15 of
induction chemotherapy. All treated patients achieved complete
remission. Patients who had evidence of minimal residual disease
(MRD) ≥0.05% at the end of the first block of treatment (day 78),
and those with MRD 0.005% to 0.05% who remained MRD-positive at any
detectable level after three additional high-risk chemotherapy
blocks, were eligible for hematopoietic stem cell transplantation
(HSCT) in first remission. Among treated patients, 19 met this
criteria, and 15 (14.2%) received HSCT. The remaining 85.8% of
patients received Sprycel plus chemotherapy for two years.
“Ph+ ALL is known to have poorer outcomes than other ALL
subtypes in both adults and children, and the availability of
treatment options is limited, particularly for young patients,”
said Jonathan Leith, Ph.D., hematology development lead,
Bristol-Myers Squibb. “For more than a decade Sprycel has been an
important treatment option for adults with Ph+ ALL, and these data
help advance our understanding of its potential in pediatric
patients.”
Study CA180-372
In the ongoing CA180-372 (NCT01460160) study, patients received
Sprycel 60 mg/m2 tablets or powder for oral suspension, once daily,
in addition to a chemotherapy regimen modelled on a
Berlin-Frankfurt-Munster high-risk backbone for two years or until
the occurrence of unacceptable toxicity.
Two patients discontinued Sprycel due to toxicity, one due to
allergy and one due to prolonged thrombocytopenia. Primary
toxicities of any causality included hematological toxicity such as
grade 3 or 4 febrile neutropenia (75.5%), sepsis (23.6%) and
bacteremia (24.5%). Non-hematologic, non-infectious grade 3 or 4
adverse events (AEs) attributed to Sprycel and reported in more
than 10% of patients were limited to elevated alanine
aminotransferase (21.7%) and aspartate transaminase (10.4%). Other
grade 3 or 4 AEs attributed to Sprycel were pleural effusion
(3.8%), edema (2.8%), hemorrhage (5.7%) and cardiac failure (0.8%).
No events of pulmonary hypertension or pulmonary arterial
hypertension were reported. Seven deaths occurred during protocol
therapy, with five patients receiving chemotherapy (three due to
sepsis, one due to pneumonia and one with unknown cause) and two,
transplant-related.
About Sprycel
Sprycel first received FDA approval in 2006 for the treatment of
adults with Philadelphia chromosome-positive (Ph+) chronic myeloid
leukemia (CML) in chronic phase (CP) who are resistant or
intolerant to prior therapy including imatinib. At that time,
Sprycel was also approved for adults with Ph+ acute lymphoblastic
leukemia (ALL) who are resistant or intolerant to prior therapy.
Sprycel is approved and marketed worldwide for these indications in
more than 60 countries.
Sprycel is also an FDA-approved treatment for adults with newly
diagnosed CP Ph+ CML, and in November 2017, Sprycel received FDA
approval for the expanded indication for treatment in pediatric
patients with CP Ph+ CML. The adult indication is approved in more
than 50 countries.
U.S. FDA-APPROVED INDICATIONS FOR
SPRYCEL ®
SPRYCEL® (dasatinib) is indicated for the treatment of
adults with:
- Newly diagnosed adults with
Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia
(CML) in chronic phase.
- Chronic, accelerated, or myeloid or
lymphoid blast phase Ph+ CML with resistance or intolerance to
prior therapy including imatinib.
- Philadelphia chromosome-positive acute
lymphoblastic leukemia (Ph+ ALL) with resistance or intolerance to
prior therapy.
- Pediatric patients with Philadelphia
chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic
phase.
IMPORTANT SAFETY
INFORMATION
Myelosuppression
Treatment with SPRYCEL is associated with severe (NCI CTCAE
Grade 3/4) thrombocytopenia, neutropenia, and anemia, which occur
earlier and more frequently in patients with advanced phase CML or
Ph+ ALL than in patients with chronic phase CML. Myelosuppression
was reported in patients with normal baseline laboratory values as
well as in patients with pre-existing laboratory abnormalities.
- In patients with chronic phase CML,
perform complete blood counts (CBCs) every 2 weeks for 12 weeks,
then every 3 months thereafter, or as clinically indicated
- In patients with advanced phase CML or
Ph+ ALL, perform CBCs weekly for the first 2 months and then
monthly thereafter, or as clinically indicated
- Myelosuppression is generally
reversible and usually managed by withholding SPRYCEL temporarily
and/or dose reduction
- In clinical studies, myelosuppression
may have also been managed by discontinuation of study therapy
- Hematopoietic growth factor has been
used in patients with resistant myelosuppression
Bleeding-Related Events
SPRYCEL can cause serious and fatal bleeding. In all CML or Ph+
ALL clinical studies, Grade ≥3 central nervous system (CNS)
hemorrhages, including fatalities, occurred in <1% of patients
receiving SPRYCEL. The incidence of Grade 3/4 hemorrhage, occurred
in 5.8% of adult patients and generally required treatment
interruptions and transfusions. The incidence of Grade 5 hemorrhage
occurred in 0.4% of adult patients. The most frequent site of
hemorrhage was gastrointestinal.
- Most bleeding events in clinical
studies were associated with severe thrombocytopenia
- In addition to causing thrombocytopenia
in human subjects, dasatinib caused platelet dysfunction in
vitro
- Concomitant medications that inhibit
platelet function or anticoagulants may increase the risk of
hemorrhage
Fluid Retention
SPRYCEL may cause fluid retention. After 5 years of follow-up in
the adult randomized newly diagnosed chronic phase CML study
(n=258), grade 3/4 fluid retention was reported in 5% of patients,
including 3% of patients with grade 3/4 pleural effusion. In adult
patients with newly diagnosed or imatinib resistant or intolerant
chronic phase CML, grade 3/4 fluid retention occurred in 6% of
patients treated with SPRYCEL at the recommended dose (n=548). In
adult patients with advanced phase CML or Ph+ ALL treated with
SPRYCEL at the recommended dose (n=304), grade 3/4 fluid retention
was reported in 8% of patients, including grade 3/4 pleural
effusion reported in 7% of patients. In pediatric patients with
chronic phase CML cases of Grade 1 or 2 fluid retention were
reported in 10.3% of patients.
- Patients who develop symptoms of
pleural effusion or other fluid retention, such as new or worsened
dyspnea on exertion or at rest, pleuritic chest pain, or dry cough
should be evaluated promptly with a chest x-ray or additional
diagnostic imaging as appropriate
- Fluid retention events were typically
managed by supportive care measures that may include diuretics or
short courses of steroids
- Severe pleural effusion may require
thoracentesis and oxygen therapy
- Consider dose reduction or treatment
interruption
Cardiovascular Events
SPRYCEL can cause cardiac dysfunction. After 5 years of
follow-up in the randomized newly diagnosed chronic phase CML trial
in adults (n=258), the following cardiac adverse reactions
occurred:
- Cardiac ischemic events (3.9% dasatinib
vs 1.6% imatinib), cardiac related fluid retention (8.5% dasatinib
vs 3.9% imatinib), and conduction system abnormalities, most
commonly arrhythmia and palpitations (7.0% dasatinib vs 5.0%
imatinib). Two cases (0.8%) of peripheral arterial occlusive
disease occurred with imatinib and 2 (0.8%) transient ischemic
attacks occurred with dasatinib
Monitor patients for signs or symptoms consistent with cardiac
dysfunction and treat appropriately.
Pulmonary Arterial Hypertension (PAH)
SPRYCEL may increase the risk of developing PAH in adult and
pediatric patients, which may occur any time after initiation,
including after more than 1 year of treatment. Manifestations
include dyspnea, fatigue, hypoxia, and fluid retention. PAH may be
reversible on discontinuation of SPRYCEL.
- Evaluate patients for signs and
symptoms of underlying cardiopulmonary disease prior to initiating
SPRYCEL and during treatment. If PAH is confirmed, SPRYCEL should
be permanently discontinued
QT Prolongation
SPRYCEL may increase the risk of prolongation of QTc in patients
including those with hypokalemia or hypomagnesemia, patients with
congenital long QT syndrome, patients taking antiarrhythmic
medicines or other medicinal products that lead to QT prolongation,
and cumulative high-dose anthracycline therapy
- Correct hypokalemia or hypomagnesemia
prior to and during SPRYCEL administration
Severe Dermatologic Reactions
Cases of severe mucocutaneous dermatologic reactions, including
Stevens-Johnson syndrome and erythema multiforme, have been
reported in patients treated with SPRYCEL.
- Discontinue permanently in patients who
experience a severe mucocutaneous reaction during treatment if no
other etiology can be identified
Tumor Lysis Syndrome (TLS)
TLS has been reported in patients with resistance to prior
imatinib therapy, primarily in advanced phase disease.
- Due to potential for TLS, maintain
adequate hydration, correct uric acid levels prior to initiating
therapy with SPRYCEL, and monitor electrolyte levels
- Patients with advanced stage disease
and/or high tumor burden may be at increased risk and should be
monitored more frequently
Embryo-Fetal Toxicity
Based on limited human data, SPRYCEL can cause fetal harm when
administered to a pregnant woman. Hydrops fetalis, fetal leukopenia
and fetal thrombocytopenia have been reported with maternal
exposure to SPRYCEL. Transplacental transfer of dasatinib has been
measured in fetal plasma and amniotic fluid at concentrations
comparable to those in maternal plasma.
- Advise females of reproductive
potential to avoid pregnancy, which may include the use of
effective contraception, during treatment with SPRYCEL and for 30
days after the final dose
Effects on Growth and Development in Pediatric Patients
In pediatric trials of SPRYCEL in chronic phase CML after at
least 2 years of treatment, adverse reactions associated with bone
growth and development were reported in 5 (5.2%) patients, one of
which was severe in intensity (Growth Retardation Grade 3). These 5
cases included cases of epiphyses delayed fusion, osteopenia,
growth retardation, and gynecomastia. Of these 5 cases, 1 case of
osteopenia and 1 case of gynecomastia resolved during
treatment.
Lactation
No data are available regarding the presence of dasatinib in
human milk, the effects of the drug on the breastfed child or the
effects of the drug on milk production. However, dasatinib is
present in the milk of lactating rats.
- Because of the potential for serious
adverse reactions in nursing children from SPRYCEL, breastfeeding
is not recommended during treatment with SPRYCEL and for 2 weeks
after the final dose
Drug Interactions
- Strong CYP3A4
inhibitors: The coadministration with strong CYP3A
inhibitors may increase dasatinib concentrations. Increased
dasatinib concentrations may increase the risk of toxicity. Avoid
concomitant use of strong CYP3A4 inhibitors. If concomitant
administration of a strong CYP3A4 inhibitor cannot be avoided,
consider a SPRYCEL dose reduction
- Grapefruit juice may
increase plasma concentrations of SPRYCEL and should be
avoided
- Strong CYP3A4 inducers: The
coadministration of SPRYCEL with strong CYP3A inducers may decrease
dasatinib concentrations. Decreased dasatinib concentrations may
reduce efficacy. Consider alternative drugs with less enzyme
induction potential. If concomitant administration of a strong
CYP3A4 inducer cannot be avoided, consider a SPRYCEL dose increase
- St. John’s wort may
decrease plasma concentrations of SPRYCEL and should be
avoided
- Gastric Acid Reducing
Agents: The coadministration of SPRYCEL with a gastric
acid reducing agent may decrease the concentrations of dasatinib.
Decreased dasatinib concentrations may reduce efficacy.Do not
administer H2 antagonists or proton pump
inhibitors with SPRYCEL. Consider the use of antacids in place of
H2 antagonists or proton pump inhibitors. Administer the
antacid at least 2 hours prior to or 2 hours after the dose of
SPRYCEL. Avoid simultaneous administration of SPRYCEL with
antacids.
Adverse Reactions
The safety data reflects exposure to SPRYCEL at all doses tested
in clinical studies (n=2809) including 324 adult patients with
newly diagnosed chronic phase CML, 2388 adult patients with
imatinib resistant or intolerant chronic or advanced phase CML or
Ph+ ALL, and 97 pediatric patients with chronic phase CML.
The median duration of therapy in a total of 2712
SPRYCEL-treated adult patients was 19.2 months (range 0–93.2
months). Median duration of therapy in:
- 1618 adult patients with chronic phase
CML was 29 months (range 0–92.9 months)
- Median duration for 324 adult patients
in the newly diagnosed chronic phase CML trial was approximately 60
months
- 1094 adult patients with advanced phase
CML or Ph+ ALL was 6.2 months (range 0–93.2 months)
In two non-randomized trials in 97 pediatric patients with
chronic phase CML (51 patients newly diagnosed and 46 patients
resistant or intolerant to previous treatment with imatinib), the
median duration of therapy was 51.1 months (range 1.9 to 99.6
months).
In the newly diagnosed adult chronic phase CML trial, after a
minimum of 60 months of follow-up, the cumulative discontinuation
rate for 258 patients was 39%.
In the overall population of 2712 adult SPRYCEL-treated
patients, 88% of patients experienced adverse reactions at some
time and 19% experienced adverse reactions leading to treatment
discontinuation.
Among the 1618 adult SPRYCEL-treated patients with chronic phase
CML, drug-related adverse reactions leading to discontinuation were
reported in 329 (20.3%) patients.
- In the adult newly diagnosed chronic
phase CML trial, drug was discontinued for adverse reactions in 16%
of SPRYCEL-treated patients with a minimum of 60 months of
follow-up
Among the 1094 SPRYCEL-treated patients with advanced phase CML
or Ph+ ALL, drug-related adverse reactions leading to
discontinuation were reported in 191 (17.5%) patients.
Among the 97 pediatric subjects, drug-related adverse reactions
leading to discontinuation were reported in 1 patient (1%).
Patients ≥65 years are more likely to experience the commonly
reported adverse reactions of fatigue, pleural effusion, diarrhea,
dyspnea, cough, lower gastrointestinal hemorrhage, and appetite
disturbance, and more likely to experience the less frequently
reported adverse reactions of abdominal distention, dizziness,
pericardial effusion, congestive heart failure, hypertension,
pulmonary edema and weight decrease, and should be monitored
closely.
- In adult newly diagnosed chronic phase
CML patients:
- Drug-related serious adverse reactions
(SARs) were reported for 16.7% of patients. Serious adverse
reactions reported in ≥5% of patients included pleural effusion
(5%)
- Grade 3/4 laboratory abnormalities
included neutropenia (29%), thrombocytopenia (22%), anemia (13%),
hypophosphatemia (7%), hypocalcemia (4%), elevated bilirubin (1%),
and elevated creatinine (1%)
- In adult patients resistant or
intolerant to prior imatinib therapy:
- Drug-related SARs were reported for
26.1% of SPRYCEL-treated patients treated at the recommended dose
of 100 mg once daily in the randomized dose-optimization trial of
patients with chronic phase CML resistant or intolerant to prior
imatinib therapy. Serious adverse reactions reported in ≥5% of
patients included pleural effusion (10%)
- Grade 3/4 hematologic laboratory
abnormalities in chronic phase CML patients resistant or intolerant
to prior imatinib therapy who received SPRYCEL 100 mg once daily
with a minimum follow up of 60 months included neutropenia (36%),
thrombocytopenia (24%), and anemia (13%). Other grade 3/4
laboratory abnormalities included: hypophosphatemia (10%), and
hypokalemia (2%)
- Among chronic phase CML patients with
resistance or intolerance to prior imatinib therapy, cumulative
grade 3/4 cytopenias were similar at 2 and 5 years including:
neutropenia (36% vs 36%), thrombocytopenia (23% vs 24%), and anemia
(13% vs 13%)
- Grade 3/4 elevations of transaminases
or bilirubin and Grade 3/4 hypocalcemia, hypokalemia, and
hypophosphatemia were reported in patients with all phases of CML
- Elevations in transaminases or
bilirubin were usually managed with dose reduction or
interruption
- Patients developing Grade 3/4
hypocalcemia during the course of SPRYCEL therapy often had
recovery with oral calcium supplementation
- In pediatric subjects with Ph+ CML in
chronic phase
- Drug-related SARs were reported for
14.4% of pediatric patients
- In the pediatric studies, the rates of
laboratory abnormalities were consistent with the known profile for
laboratory parameters in adults
- Most common adverse reactions (≥15%) in
patients included myelosuppression, fluid retention events,
diarrhea, headache, skin rash, hemorrhage, dyspnea, fatigue,
nausea, and musculoskeletal pain
Please see full Prescribing Information
here.
About Bristol-Myers
Squibb
Bristol-Myers Squibb is a global biopharmaceutical company whose
mission is to discover, develop and deliver innovative medicines
that help patients prevail over serious diseases. For more
information about Bristol-Myers Squibb, visit us at BMS.com or
follow us on LinkedIn, Twitter, YouTube and Facebook.
Bristol-Myers Squibb Forward-Looking Statement
This press release contains "forward-looking statements" as that
term is defined in the Private Securities Litigation Reform Act of
1995 regarding the research, development and commercialization of
pharmaceutical products. Such forward-looking statements are based
on current expectations and involve inherent risks and
uncertainties, including factors that could delay, divert or change
any of them, and could cause actual outcomes and results to differ
materially from current expectations. No forward-looking statement
can be guaranteed. Among other risks, there can be no guarantee
that Sprycel will receive regulatory approval for an additional
indication described herein. Forward-looking statements in this
press release should be evaluated together with the many
uncertainties that affect Bristol-Myers Squibb's business,
particularly those identified in the cautionary factors discussion
in Bristol-Myers Squibb's Annual Report on Form 10-K for the year
ended December 31, 2016 in our Quarterly Reports on Form 10-Q and
our Current Reports on Form 8-K. Bristol-Myers Squibb undertakes no
obligation to publicly update any forward-looking statement,
whether as a result of new information, future events or
otherwise.
View source
version on businesswire.com: http://www.businesswire.com/news/home/20171209005074/en/
Bristol-Myers Squibb CompanyMedia:Audrey Abernathy, cell:
919-605-4521audrey.abernathy@bms.comorInvestor:Bill
Szablewski, 609-252-5894william.szablewski@bms.comorTim Power,
609-252-7509timothy.power@bms.com
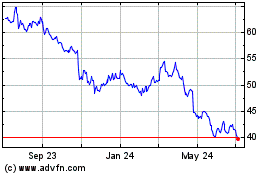
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
From Mar 2024 to Apr 2024
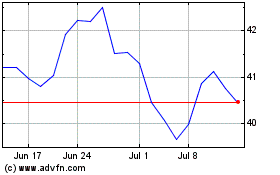
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
From Apr 2023 to Apr 2024