Judge Blocks Rule That Could Limit Premium Assistance for Dialysis Patients
January 12 2017 - 10:32PM
Dow Jones News
By Anna Wilde Mathews
A judge blocked a federal rule that was expected to limit
dialysis providers' ability to help patients pay for individual
insurance plans, which was set to go into effect Friday.
U.S. District Judge Amos Mazzant, in Sherman, Texas, issued a
temporary restraining order delaying the rule by two weeks,
granting a request that was part of a suit filed by major dialysis
providers and a patient group. The plaintiffs, which included
DaVita Inc. and Fresenius Medical Care North America, a subsidiary
of a German company, argued that the Department of Health and Human
Services had improperly rushed out the rule and that it could hurt
patients.
The order puts the fate of the rule into question, because the
incoming Trump administration's stance on it isn't clear.
A spokesman for the Department of Health and Human Services said
officials there were "disappointed the court temporarily stayed
implementation of this important rule while scheduling further
proceedings to consider the parties' positions." A spokesman for
DaVita said the ruling was "good news for the thousands of patients
who would be harmed by the implementation of the rule."
In granting the dialysis providers' request, the judge said that
the plaintiffs had shown that the federal agency "likely violated
the procedures" of a law governing the issuance of federal
regulations. The order also said that the rule might hurt patients
by causing them "to shift to public insurance options, and many
patients would be better served by private insurance options."
The federal rule at issue would likely have affected a
controversial setup in which a nonprofit, the American Kidney Fund,
runs a program, using funding from dialysis providers, that helps
pay premiums for kidney-failure patients. That setup is being
investigated by the Boston U.S. attorney's office. In the past, the
nonprofit has said it operates its program with the "highest
integrity" and adheres to guidelines laid out by an advisory
opinion from the Office of the Inspector General of the Department
of Health and Human Services.
In the Health and Human Services rule, the agency said dialysis
providers have a "strong financial incentive...to use premium
payments to steer as many patients as possible to commercial plans"
such as the individual coverage sold under the Affordable Care Act.
The rule said the companies are paid more for their services when
patients are insured that way, rather than through government
programs such as Medicare and Medicaid.
The federal regulator said patients sometimes had problems when
they enrolled in the individual insurance plans, facing potentially
higher costs and disruption if an insurer decided to stop accepting
their third-party premium support, and the rule needed to take
effect quickly to avoid further harm to patients.
The rule would require dialysis providers to tell insurers when
their patients are getting help from the providers, directly or
indirectly, to pay premiums for individual insurance plans. The
providers are also supposed to get assurances the insurer will
accept those payments. The federal agency estimated that around
7,000 dialysis patients get premium help for individual health
plans either directly or indirectly from dialysis companies.
Analysts have said insurers would likely often refuse the
payments, with the result that some patients wouldn't be able to
enroll in the individual plans. They have said that a loss of
commercially insured patients could hurt earnings at dialysis
companies.
Write to Anna Wilde Mathews at anna.mathews@wsj.com
(END) Dow Jones Newswires
January 12, 2017 22:17 ET (03:17 GMT)
Copyright (c) 2017 Dow Jones & Company, Inc.
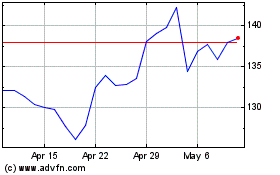
DaVita (NYSE:DVA)
Historical Stock Chart
From Mar 2024 to Apr 2024
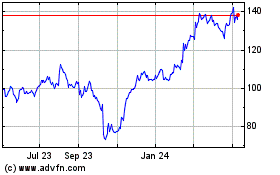
DaVita (NYSE:DVA)
Historical Stock Chart
From Apr 2023 to Apr 2024