CVS Drops Coverage of 2 Branded Biotech Drugs in Favor of Copies
August 02 2016 - 7:30PM
Dow Jones News
CVS Health Corp. is embracing new, cheaper copies of biotech
medicines in an attempt to combat rising prescription drug
costs.
CVS, whose Caremark unit administers drug-benefit plans for
employers and insurers, said Tuesday it would drop coverage of two
higher-priced medicines used in diabetes and cancer treatments. It
will instead cover their replica versions, sometimes called
biosimilars, for many of its drug-plan members.
The changes, which go into effect Jan. 1, are a blow to Sanofi
SA's Lantus, a popular brand-name insulin treatment for diabetes,
and Amgen Inc.'s Neupogen, which helps to prevent infections
related to cancer treatment. A vial of Lantus retails for about
$260 while a single dose of Neupogen costs about $350, according to
GoodRx.
Cheaper copies of biotech drugs have only recently begun to
enter the U.S. market and haven't yet made much of a dent in the
nation's drug spending, in part because they have been priced at
relatively small discounts to their branded rivals.
But the move by CVS is the latest indication that U.S. health
insurers and pharmacy benefit managers are eager to reap savings
from the new drugs. CVS Chief Medical Officer Troyen A. Brennan
said biosimilars are typically priced 10% to 15% cheaper but that
CVS has negotiated additional discounts.
"We want to signal that this biosimilar movement is real," Dr.
Brennan said in an interview. "We have big hopes for [biosimilars]
to reduce drug costs over all."
An Amgen spokeswoman said Neupogen "is competitively priced,"
and that patients and doctors should be able to choose which
product they want to use. A Sanofi spokesman said CVS's decision to
exclude Lantus and another of the company's insulins would make "it
difficult for patients to benefit from the gold standard of basal
insulin treatment."
CVS, best known as a retail pharmacy chain, is also a major
player in the pharmacy benefit management industry, overseeing drug
spending for U.S. employers, health insurers and labor unions. CVS
and other PBMs pool their customers' purchasing power to negotiate
better prices from drugmakers. In exchange, PBMs often steer their
clients to products for which they receive the best prices. Last
year, CVS dropped coverage for Pfizer Inc.'s anti-impotence pill
Viagra in favor of Eli Lilly & Co.'s Cialis.
However, the exclusions aren't ironclad. Some PBM clients
customize their own covered-drug lists, and many prefer to give
beneficiaries as many options as possible. The changes that CVS
announced on Tuesday, for instance, will apply mainly to its
commercial employer and labor union clients who subscribe to its
standard formulary, or list of covered drugs.
CVS said it would exclude an additional 35 products in 2017,
including Novartis AG's cancer drugs Gleevec and Tasigna. A generic
version of Gleevec was launched earlier this year. CVS's Dr.
Brennan said the company intends to have all patients currently
taking Gleevec switched to the generic version.
A Novartis spokesman said the company was disappointed that CVS
would limit access to Tasigna, but that CVS had indicated the
coverage decision wouldn't "affect any patients who are currently
taking Tasigna."
Write to Joseph Walker at joseph.walker@wsj.com and Paul Ziobro
at Paul.Ziobro@wsj.com
(END) Dow Jones Newswires
August 02, 2016 19:15 ET (23:15 GMT)
Copyright (c) 2016 Dow Jones & Company, Inc.
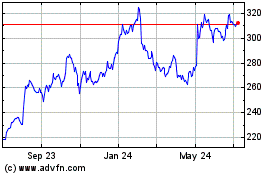
Amgen (NASDAQ:AMGN)
Historical Stock Chart
From Mar 2024 to Apr 2024
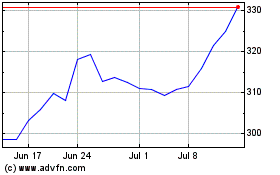
Amgen (NASDAQ:AMGN)
Historical Stock Chart
From Apr 2023 to Apr 2024